HLA-DQ Mismatches Are More Likely to Be Listed as Unacceptable Antigens After Renal Graft Failure in African American Recipients as Compared to Other Racial/Ethnic Groups
1Northwestern University, Chicago, IL, 2London School of Economics, London, United Kingdom, 3Cambridge University, Cambridge, United Kingdom, 4Cleveland Clinic, Cleveland, OH
Meeting: 2022 American Transplant Congress
Abstract number: 511
Keywords: African-American, Graft failure, Hispanic, HLA matching
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Name: Health Equity and Access II
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:00pm-6:10pm
Presentation Time: 6:00pm-6:10pm
Location: Hynes Ballroom C
*Purpose: Growing evidence suggests that donor-recipient mismatches at the HLA-DQ locus are the most immunogenic and pathogenic, evidenced by generation of DQ donor-specific antibodies (DSA). Racial/ethnic minorities in the US have less access to HLA-matched kidneys and experience greater sensitization after graft loss, however the contribution of DQ DSA in these populations is not well characterized. Data in the Scientific Registry of Transplant Recipients (SRTR) do not include DSA, preventing direct study of DQ DSA and transplant outcomes. Given this limitation, we apply a novel approach focusing on patients in the SRTR who lost their initial graft and were relisted with new unacceptable antigens (UA) corresponding to donor HLA type. The appearance of UA after graft loss suggests that the mismatches contributed to graft failure. Here we utilize this metric to assess the effect of HLA-DQ on graft failure in different racial/ethnic groups.
*Methods: Adult patients in the SRTR who received a primary kidney transplant from 1/1/2010 – 3/1/2020 and were relisted after graft failure were included if they had donor/recipient typing and UA data available at the HLA-A, B, C, DR and DQ loci. Multiple linear regression was applied to evaluate: 1) the probability of donor HLA mismatches being recorded as new UA after relisting, 2) the likelihood that HLA-DQ was designated as an UA as compared to other HLA loci and 3) the comparative probabilities of developing a donor-specific DQ UA in African American, White and Hispanic recipients.
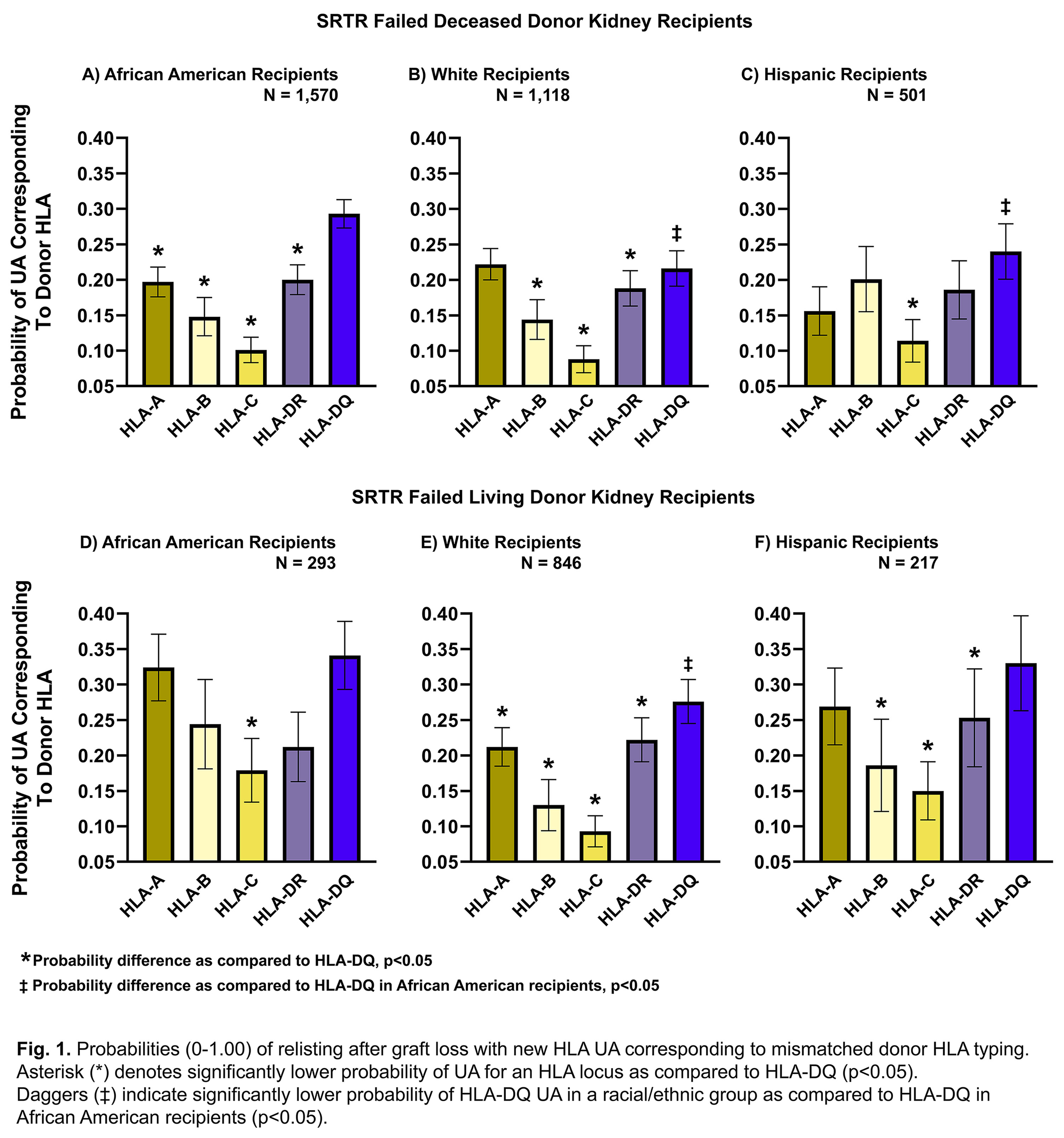
*Results: 3,189 deceased donor and 1,356 living donor recipients were included. Overall, DQ mismatches resulted in a higher probability of donor-specific UA as compared to all other HLA loci (p<0.05). Results by recipient race/ethnicity are depicted in Fig. 1. After a failed deceased donor kidney, African American recipients were more likely to be relisted with new DQ UA as compared to White and Hispanic recipients (p<0.05). After a failed living donor kidney, African American and Hispanic recipients were more likely to be relisted with new DQ UA as compared to White recipients (p<0.05).
*Conclusions: HLA-DQ mismatches produce disproportionately higher rates of UA after graft failure compared to other HLA loci. This effect is most pronounced in African American recipients. Future changes to kidney allocation priority should consider the effects of HLA-DQ matching on equity.
To cite this abstract in AMA style:
Isaacson D, Gmeiner MW, Kosmoliaptsis V, Schold JD, Tambur AR. HLA-DQ Mismatches Are More Likely to Be Listed as Unacceptable Antigens After Renal Graft Failure in African American Recipients as Compared to Other Racial/Ethnic Groups [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/hla-dq-mismatches-are-more-likely-to-be-listed-as-unacceptable-antigens-after-renal-graft-failure-in-african-american-recipients-as-compared-to-other-racial-ethnic-groups/. Accessed March 8, 2026.« Back to 2022 American Transplant Congress