Resource Expenditure in the Evaluation of Older Donors for Heart Transplant: An Impediment to Donor Pool Expansion?
1Stanford University School of Medicine, Stanford, CA, 2Kaiser Permanente Northern California, Oakland, CA, 3University of Wisconsin School of Medicine, Madison, WI, 4Donor Network of Arizona, Tempe, AZ, 5LifeGift, Houston, TX, 6Emory University School of Medicine, Atlanta, GA, 7Gift of Life Michigan, Ann Arbor, MI
Meeting: 2022 American Transplant Congress
Abstract number: 438
Keywords: Donors, marginal, Economics, Heart, Organ Selection/Allocation
Topic: Clinical Science » Organ Inclusive » 68 - Deceased Donor Management and Intervention Research
Session Information
Session Name: Surgical Issues: Donor and Recipient
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:50pm-4:00pm
Presentation Time: 3:50pm-4:00pm
Location: Hynes Room 310
*Purpose: Using older donors for heart transplant (HT) could alleviate donor scarcity but the resource implications of this strategy – and whether evaluation of older donors is more costly – should be assessed. We did so using data from the Donor Heart Study (DHS).
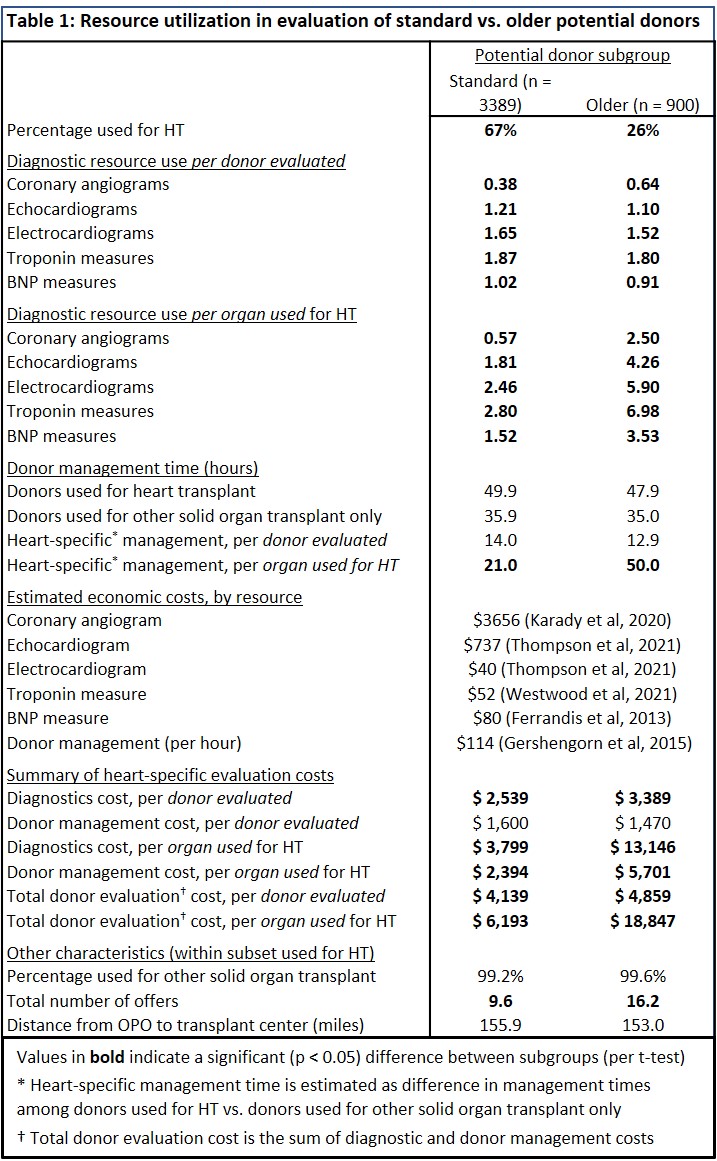
*Methods: The DHS enrolled potential donors at 8 organ procurement organizations in the United States (US) in 2015 – 2020. We included only those receiving a screening echocardiogram – indicating that they were evaluated for potential HT. We compared resource expenditure – both per potential donor and per organ used for HT – for “standard” (age < 50 years) and “older” (age ≥ 50) donors in this cohort. We considered only heart specific diagnostics and donor management time – that which would vary depending on consideration for HT (vs. other solid organ transplant only). We expressed each resource in economic terms and calculated total cost per organ used.
*Results: 3389 standard and 900 older donors were evaluated for HT; among these 67% of standard and 26% of older potential donor hearts were used for HT. Per donor evaluated, older (vs. standard) donors had slightly higher diagnostic costs but similar donor management time. But on a per organ used basis, older potential donors had higher heart specific donor management time (50 vs. 21 hours) and more angiograms (2.5 vs. 0.6), echocardiograms (4.2 vs.1.8), electrocardiograms (5.9 vs. 2.5), and troponin (6.9 vs. 2.8) and β-type natriuretic peptide (3.5 vs. 1.5) measures. In economic terms (per organ used for HT), this equates to diagnostic costs of $3,797 for standard and $13,021 for older donors and donor management costs of $2,394 for standard and $5,701 for older donors.
*Conclusions: Older potential donors are less likely to be accepted for HT and (as a result) incur higher (per HT) evaluation costs. This additional cost (~$13k) is tiny compared to the total system level cost per HT (> $1 million); thus it should not reduce the cost-effectiveness of HT (relative to alternative therapies) or impede necessary efforts to expand the donor pool. But on a local level, this $13k is a burden that could induce unduly conservative selection of potential donors. Evidence-based policy and incentives to guide screening and increase acceptance of older donors for HT could mitigate this burden.
To cite this abstract in AMA style:
Wayda B, Zaroff JG, Neidlinger N, Geraghty P, Wood RP, Nieto J, Pearson TC, Nicely B, Khush KK. Resource Expenditure in the Evaluation of Older Donors for Heart Transplant: An Impediment to Donor Pool Expansion? [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/resource-expenditure-in-the-evaluation-of-older-donors-for-heart-transplant-an-impediment-to-donor-pool-expansion/. Accessed January 30, 2026.« Back to 2022 American Transplant Congress