Spectrum of Pre-Transplant Esophagram Abnormalities and Association with Long-Term Outcomes
1University of Texas - Southwestern, Dallas, TX, 2Department of Internal Medicine, Division of Pulmonary and Critical Care Medicine, University of Texas - Southwestern, Dallas, TX, 3Cardiovascular & Thoracic Surgery, University of Texas - Southwestern, Dallas, TX
Meeting: 2022 American Transplant Congress
Abstract number: 1490
Keywords: Length of stay, Lung transplantation, Mortality, Multivariate analysis
Topic: Clinical Science » Lung » 64 - Lung: All Topics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: To determine the frequency and type of esophageal abnormalities on screening esophagram during the pre-transplant evaluation and evaluate the association of these abnormalities on early and late outcomes.
*Methods: We reviewed our institutional database for all the patients who underwent single or bilateral lung transplantation (LT) between Jan 1, 2012 to November 30, 2016 (n=324). Among these, 24 patients who did not have a pre-transplant esophagram were excluded (final N=300; mean age: 56.3±13.1 yrs, M:F 174:126, mean LAS at match 47.7±16.9). Patients were classified into four groups based on the findings on the esophagram (normal, n=159; reflux, n=70; dysmotility, n=48; and reflux with dysmotility, n=23). Variables were compared among groups based upon the esophagram findings. All patients completed 5-year post-transplant follow-up and post-transplant survival was primary outcome variable.
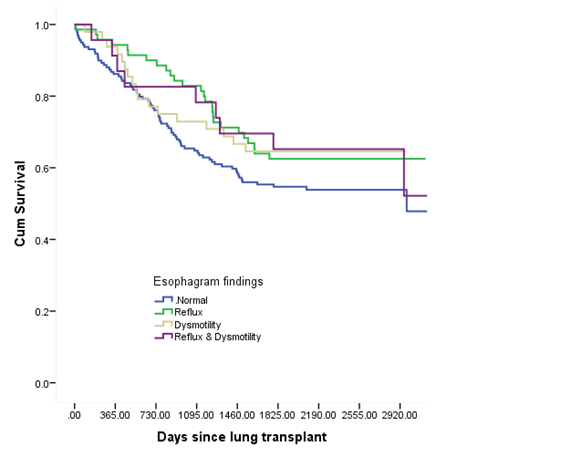
*Results: Esophagram abnormalities were common (47%) with reflux alone being the most common (23.3%) followed by dysmotility (13.3%). Transplant indication was strongly associated with esophagram findings (p<0.001) of dysmotility, with or without reflux, being most frequent among patients with restrictive lung diseases (34.7% vs 9.8%; OR: 95% CI: 4.9, 2.6-9.5; p<0.001). No other baseline variables including lung allocation score were associated with esophagram findings. Early outcomes such as primary graft dysfunction, post-operative acute kidney injury, length of hospital stay and hospital survival after LT were similar among the four groups. Furthermore, esophagram findings did not predict CLAD-free survival at three years or five-year post-LT survival (KM survival analysis in the Figure). On Cox proportional hazards model, esophagram findings did not have an independent association with post-LT survival (p=0.347)
*Conclusions: Pre-transplant esophagram abnormalities are common. Patients with reflux and/or dysmotility on esophagram do not experience worse early or late post-transplant outcomes.
To cite this abstract in AMA style:
Lill I, Lovin D, Lawrence AC, Mohanka M, Joerns J, Bollineni S, Timofte IL, Kaza V, Wait M, Torres F, Banga A. Spectrum of Pre-Transplant Esophagram Abnormalities and Association with Long-Term Outcomes [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/spectrum-of-pre-transplant-esophagram-abnormalities-and-association-with-long-term-outcomes/. Accessed February 28, 2026.« Back to 2022 American Transplant Congress