Immunosuppressants Alter Lymph Node Architecture and Create Distinct Microbiome Footprints
1University of Maryland School of Medicine, Baltimore, MD, 2University of Maryland, Baltimore, MD
Meeting: 2022 American Transplant Congress
Abstract number: 1280
Keywords: FTY720 immunosuppressant, Immunosuppression, Lymph node, Mycophenolate mofetil
Topic: Basic Science » Basic Science » 12 - Immunosuppression & Tolerance: Preclinical & Translational Studies
Session Information
Session Name: Immunosuppression & Tolerance: Preclinical & Translational Studies
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: There are complex interactions among immunosuppressants, antibiotics, and the gut microbiome on the host immune system. Microbiota can alter lymph node (LN) structure and immunosuppressants can alter microbiota communities; however, the interplay of immunosuppressants and microbiota on LN structure and immune cell homing is unknown. We investigated the individual contributions immunosuppressants impart on immune responses, LN architecture, gut barrier function, and gut microbiome.
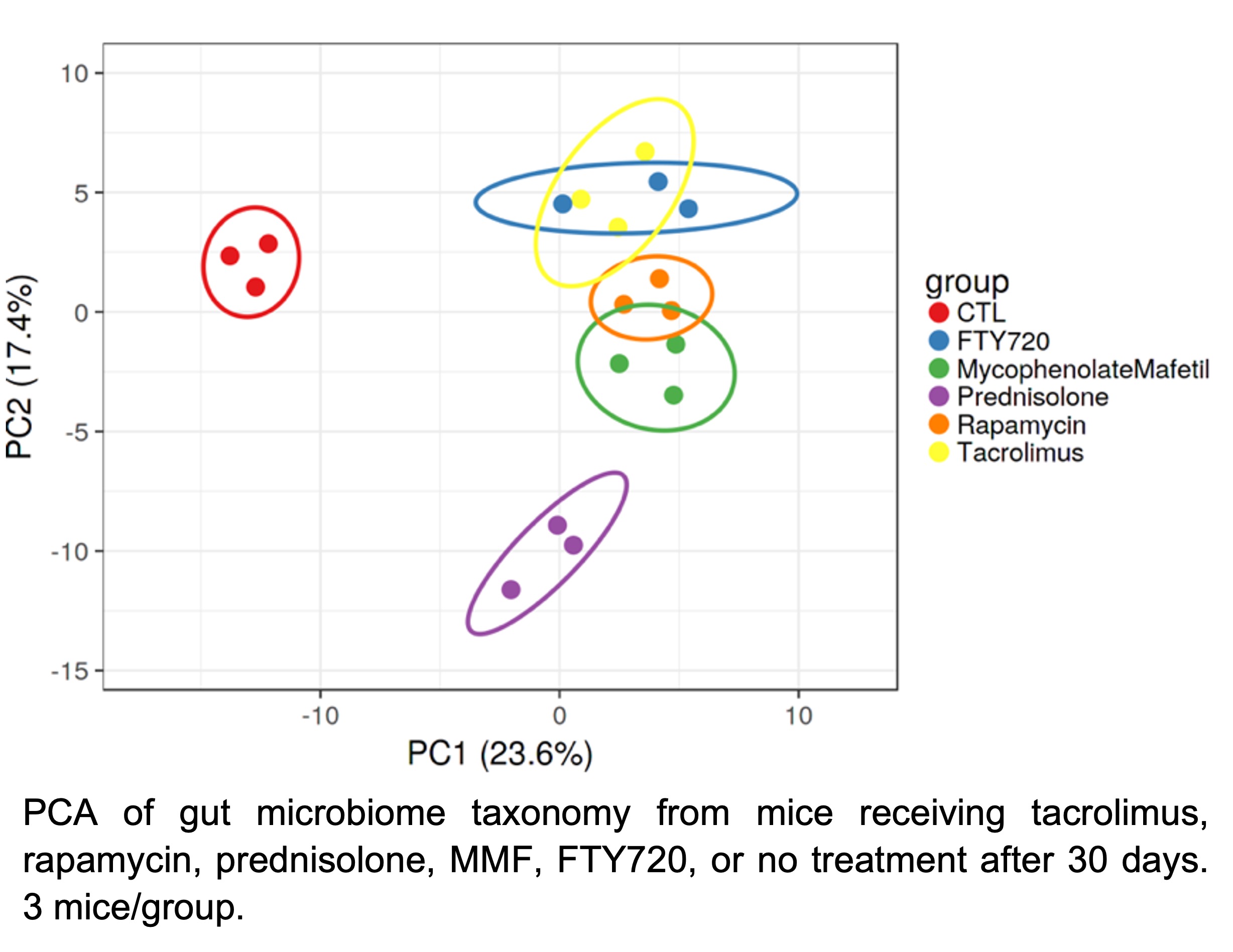
*Methods: C57BL/6 mice were treated with tacrolimus, rapamycin, prednisolone, mycophenolate mofetil (MMF), FTY720, or no treatment for 7 or 30 days. Intestinal permeability (IP) was assessed by serum analysis 4 hours after FITC-dextran gavage. Peripheral and mesenteric LN (pLN, mLN) were assessed by immunohistochemistry. Gut microbiome taxonomic composition was established from whole community metagenomic sequencing of stool. Multivariant data was mapped and visualized using the comprehensive mouse gut metagenome catalogue and principal component analysis (PCA).
*Results: MMF resulted in pro-inflammatory changes in mLN cortical ridge with decreased laminin α4:α5 ratios (p<0.0001) and increased dendritic cells (DCs) around mLN high endothelial venules (HEVs) after 7 days (p=0.0001). Prednisolone induced tolerogenic changes with increased laminin α4:α5 ratios around mLN HEVs (p<0.001) and throughout pLN (p<0.0006) after 7 days. Both FTY720 and MMF increased IP (p<0.003 and 0.03, respectively) after 7 days. Gut microbiome taxonomy of all treatment groups distinctively diverged after 30 days (Figure).
*Conclusions: MMF altered intestinal barrier function, increased DC mLN homing, and induced pro-inflammatory LN architectural changes, which may contribute to gastrointestinal MMF toxicity. Sphingosine 1-Phosphate receptor agonism (FTY720) increased IP, possibly interfering with immunosuppressant actions. Prednisolone induced anti-inflammatory LN architecture, correlating with its suppressive effects. Each immunosuppressant differentially affected the gut microbiome, a therapeutic fingerprint that may reflect alterations in mucosal immunologic homeostasis, gut metabolism, and immunosuppressive efficacy, an underappreciated consequence of these drugs.
To cite this abstract in AMA style:
Gavzy SJ, Lakhan R, Iyyathurai J, Saxena V, Li L, Ma B, Mongodin E, Bromberg JS. Immunosuppressants Alter Lymph Node Architecture and Create Distinct Microbiome Footprints [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/immunosuppressants-alter-lymph-node-architecture-and-create-distinct-microbiome-footprints/. Accessed February 9, 2026.« Back to 2022 American Transplant Congress