Increased Plasminogen Activator Inhibitor-1 is Associated with Less Severe Clinical Bleeding After Reperfusion During Liver Transplantation
University of California, San Francisco, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 1512
Keywords: Endothelial cells, Surgery
Topic: Clinical Science » Organ Inclusive » 71 - Surgical Issues (Open, Minimally Invasive):All Organs
Session Information
Session Name: Surgical Issues (Open, Minimally Invasive): All Organs
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Severe bleeding following reperfusion in liver transplantation (LT) is often discrepant with available objective laboratory and thromboelastography data. This bleeding may be due to ischemia reperfusion injury (IRI), however the severity of IRI after LT is graded by peak AST levels within 48 hours and therefore provides little intraoperative utility. “Cold IRI” is initiated by damage to endothelial cells within the liver during cold storage. This investigation examined biomarkers associated with coagulation and endothelial cells to determine whether any circulating factors might contribute to severe bleeding following reperfusion.
*Methods: We analyzed data obtained for the Mild Hypothermia and Acute Kidney Injury in Liver Transplantation trial (MHALT) which randomized patients to mild hypothermia or normothermia during the implantation phase of LT. Pre-, peri-, and post-operative clinical variables were obtained. Peripheral blood was obtained prior to incision, and two hours following portal reperfusion. The attending surgeon assessed bleeding severity 30 minutes following arterial reperfusion. Concentrations of thrombomodulin (TM), tissue factor (TF), and plasminogen activator inhibitor 1 (PAI-1) were quantified. The cohort was analyzed according to bleeding severity; continuous variables were compared with Mann-Whitney U test and categorical via Fisher exact test. Significance was set at p<0.05.
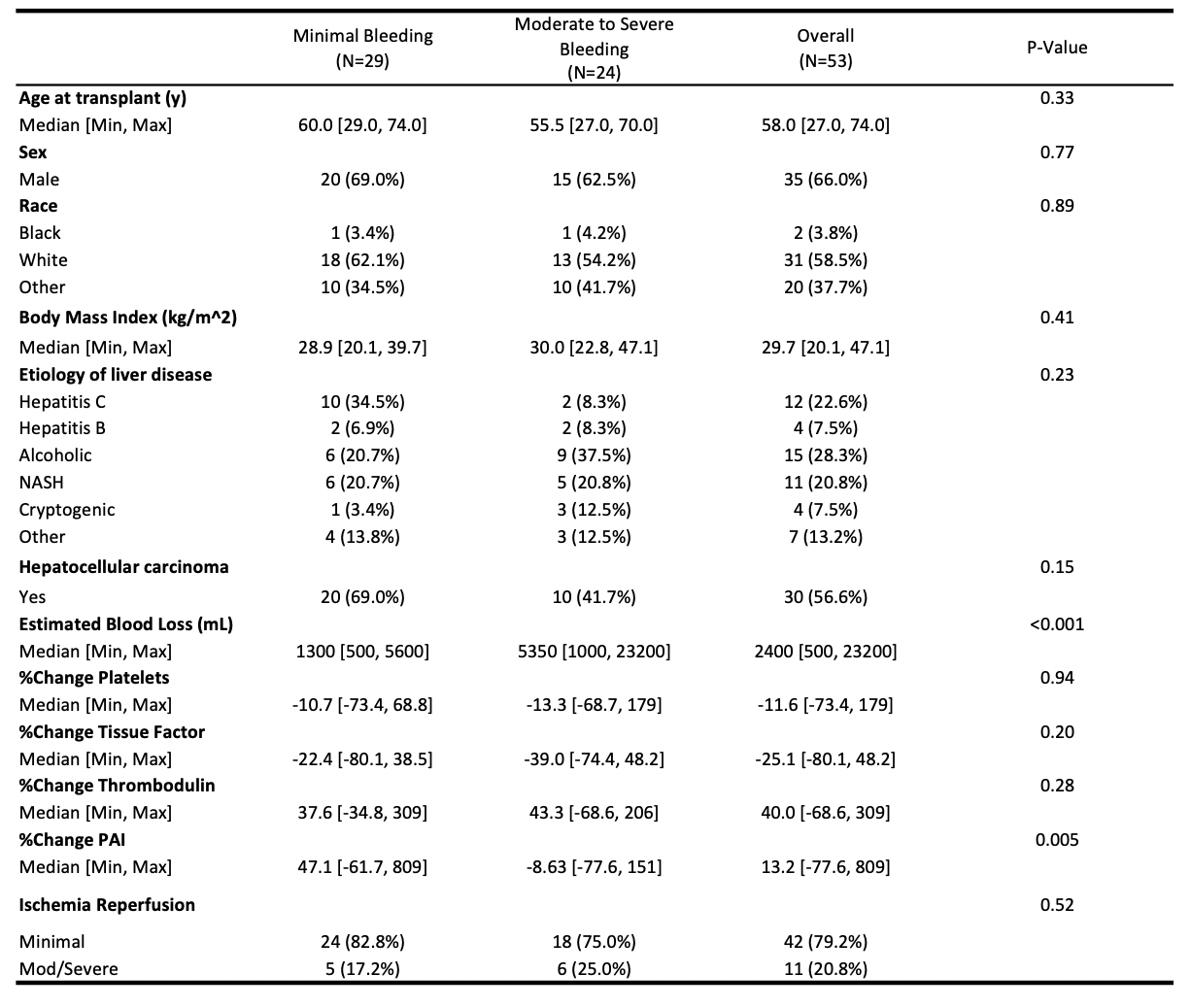
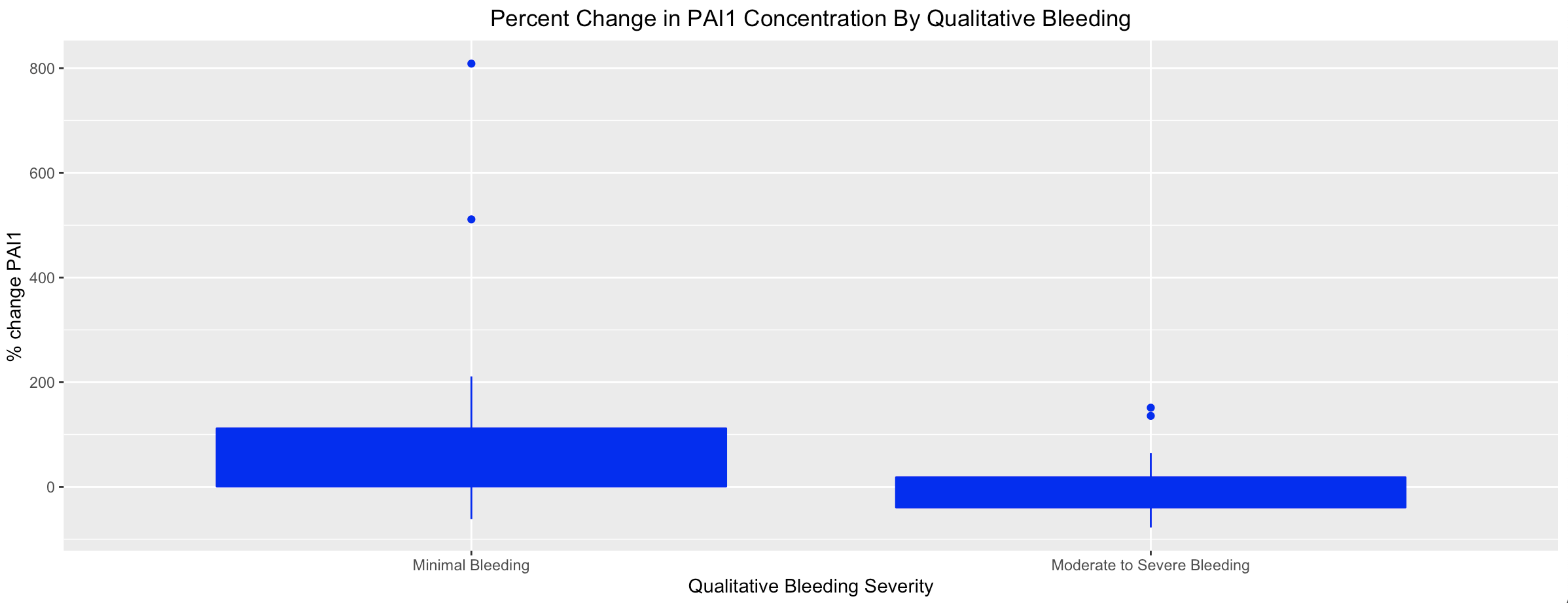
*Results: 65 patients were enrolled in MHALT; 53 had qualitative assessments of bleeding. Pre- and intra-operative demographic data by bleeding severity is shown in Figure 1. There were no differences in percent change of TM or TF before/after reperfusion, however those with minimal bleeding had a significantly greater percent increase in PAI-1 concentration following reperfusion compared to those with moderate/severe bleeding (p=0.005, Figure 2).
*Conclusions: Increased PAI-1 concentration is associated with less severe bleeding following reperfusion during LT. This suggests that the clinically significant bleeding not explained by traditional laboratory tests may be the result of dysregulation of fibrinolysis homeostasis.
To cite this abstract in AMA style:
Braun HJ, Ascher N, Roll G, Roberts J, Niemann C, Bokoch M. Increased Plasminogen Activator Inhibitor-1 is Associated with Less Severe Clinical Bleeding After Reperfusion During Liver Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/increased-plasminogen-activator-inhibitor-1-is-associated-with-less-severe-clinical-bleeding-after-reperfusion-during-liver-transplantation/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress