A Single Center Retrospective Cohort Study Comparing the Rates of MDROs in DCD vs DBD Liver Transplant Recipients
J. Walker, C. Bennett, R. Griffin, B. Orandi, J. Locke, R. Cannon, S. Sheikh, A. Nellore, R. Lee
University of Alabama at Birmingham, Birmingham, AL
Meeting: 2022 American Transplant Congress
Abstract number: 359
Keywords: Infection, Liver transplantation
Topic: Clinical Science » Infection Disease » 24 - All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: Transplant Infectious Diseases: All Organs
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:50pm-7:00pm
Presentation Time: 6:50pm-7:00pm
Location: Hynes Ballroom B
*Purpose: Donation after cardiac death (DCD) offers an opportunity to reduce wait list mortality with similar 5-year graft survival rates to donation after brain death (DBD). However, concern for increased risk of allograft dysfunction and ischemic cholangiopathy after receipt of DCD organs remain. These are among many factors that have been identified to increase risk for multi-drug resistant organisms (MDRO) infections, a significant cause of morbidity and mortality post transplant. The primary objective of this study was to determine if there is an increase incidence of MDRO infections following LT from DCD versus DBD.
*Methods: We designed a retrospective cohort study of all patients who underwent LT at UAB Hospital between Jan 2014 and December 2020. We collected variables previously associated with increased infection risk in the LT population: BMI, intraoperative transfusions, history of prior infection, and cold ischemia time (CIT). Infectious event was defined by positive culture from serum, intra-abdominal, or surgical site infection. MDRO pathogens were defined as gram negatives with resistance to three drug classes, methicillin resistant Staphylococcus aureus, or vancomycin resistantEnterococcus. Two investigators adjudicated these definition by medical record review. Additional variables were pulled from medical record or United Network for Organ Sharing. A chi squared test was performed to investigate an association between donor type and presence of MDRO pathogens at 90 days. Multivariable logistic regression analyses were performed to calculate adjusted odds ratios for outcomes of interest.
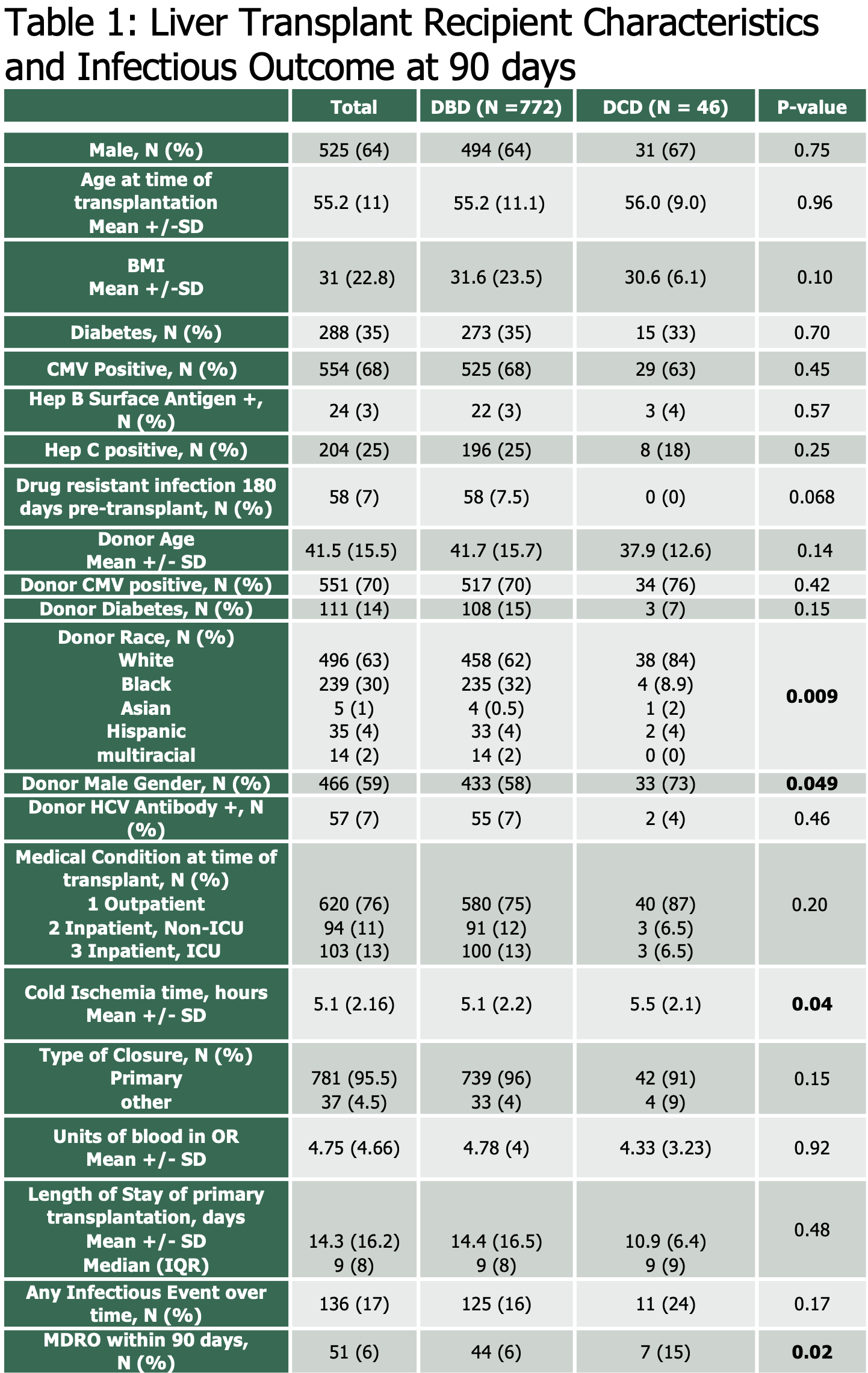
*Results: Of 818 LT recipients, 46 (5.6%) were DCD recipients. Both recipient types had similar BMI, intraoperative transfusion requirements, and diabetes (table 1). DCD LT recipients had longer CIT, though none had recent MDRO infections prior to transplant. There was no difference in infection with any organism. We found an increased risk of MDRO infections within 90 days post-transplant. When adjusted for BMI, cold ischemia time, and units of blood received in the OR, patients who received a DCD transplant were more likely to have an MDRO infection within 90 days (aOR 3.16 (1.32-7.54).
*Conclusions: Our data demonstrates an increased risk of MDRO infections following receipt of DCD organs, even after adjustment for previously identified risk factors. This should prompt vigilant post-op surveillance and consideration of mitigation strategies.
To cite this abstract in AMA style:
Walker J, Bennett C, Griffin R, Orandi B, Locke J, Cannon R, Sheikh S, Nellore A, Lee R. A Single Center Retrospective Cohort Study Comparing the Rates of MDROs in DCD vs DBD Liver Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/a-single-center-retrospective-cohort-study-comparing-the-rates-of-mdros-in-dcd-vs-dbd-liver-transplant-recipients/. Accessed February 14, 2026.« Back to 2022 American Transplant Congress