Post-Transplant Outcomes and Financial Burden in Donation After Cardiac Death Donor Liver Transplant After the Implementation of Acuity Circle Allocation Policy
Division of Transplant and Hepatobiliary Surgery, Henry Ford Hospital, Detroit, MI
Meeting: 2022 American Transplant Congress
Abstract number: 266
Keywords: Allocation, Donors, non-heart-beating, Liver transplantation
Topic: Clinical Science » Public Policy » 21 - Non-Organ Specific: Public Policy & Allocation
Session Information
Session Name: Non-Organ Specific: Public Policy & Allocation
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:20pm-4:30pm
Presentation Time: 4:20pm-4:30pm
Location: Hynes Room 311
*Purpose: The use of donation after cardiac death (DCD) donor liver grafts has been increasing in many transplant centers after introducing the acuity circles (AC) policy. The aims of this study are to compare post-liver transplant (LT) outcomes and cost between DCD and donation after brain death donor (DBD)-LT and to evaluate the impact of the AC policy on the DCD-LT practice.
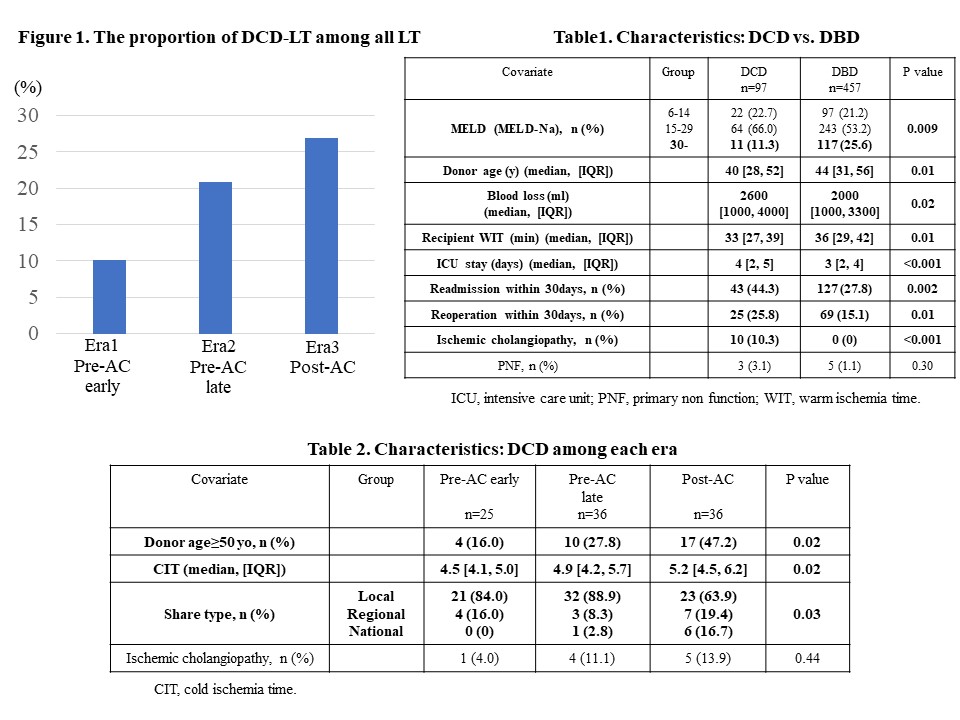
*Methods: Adult LT patients between Jan 2015 and Sep 2021 were evaluated at our center. Patients were classified into three eras: Era1 (2015-2017 [pre-AC early]), Era2 (2018-Feb 3, 2020 [pre-AC late]), and Era3 (Feb 4, 2020-Sep 2021 [post-AC]). 1) Patient characteristics, post-LT outcomes and cost were compared between DCD and DBD-LT. 2) DCD-LTs were compared between eras for the abovementioned outcomes.
*Results: A total of 97 and 457 patients with DCD and DBD-LT were evaluated. 1) The number of patients with DCD-LT in Eras 1, 2, and 3 were 25, 36, and 36, and the proportion of DCD-LT among all LTs has increased over time (Era 1 10.1%, Era 2 20.8%, Era 3 26.9%, P<0.001) (Figure 1). Compared with DBD-LT, DCD-LT recipients had lower proportion of MELD score≥30, younger donor, higher blood loss, longer ICU stay, higher readmission and reoperation rates within 30 days, and higher incidence of ischemic cholangiopathy (Table 1). Total direct, surgery, and ICU costs were higher in DCD-LT than DBD-LT ($144,158 vs. $133,591, P<0.001, $111,493 vs. $106,166, P<0.001, $3,710 vs. $2,906, P=0.002, respectively). 2) DCD-LT in Era 3 had significantly higher proportion of donor age≥50yo, more national share, and longer cold ischemia time (CIT). The incidence of ischemic cholangiopathy was higher in each successive era, though this difference did not reach statistical significance (Table 2). Total direct and surgery costs increased over time ($134,149 in Era 1 vs. $138,415 in Era 2 vs. $150,820 in Era 3, P=0.03; $100,583 in Era1 vs. $118,148 in Era2 vs. $122,404 in Era3, P<0.001, respectively). DCD-LT using donors≥50yo showed significantly higher total direct, surgery, and ICU costs than those<50yo ($154,582 vs. $138,142, P=0.01, $122,099 vs. $109,478, P=0.01, $5,921 vs. $3,492, P=0.02, respectively).
*Conclusions: The proportion of DCD-LT, especially those from older donors, became higher after introducing the AC policy. The increasing national share might lead to longer CIT. These changes were likely to be associated with the worse post-LT outcome and higher financial burden in DCD-LT in the recent era.
To cite this abstract in AMA style:
Shimada S, Shamaa T, Ivanics T, Kitajima T, Adhnan M, Collins K, Rizzari M, Yoshida A, Abouljoud M, Nagai S. Post-Transplant Outcomes and Financial Burden in Donation After Cardiac Death Donor Liver Transplant After the Implementation of Acuity Circle Allocation Policy [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/post-transplant-outcomes-and-financial-burden-in-donation-after-cardiac-death-donor-liver-transplant-after-the-implementation-of-acuity-circle-allocation-policy/. Accessed February 12, 2026.« Back to 2022 American Transplant Congress