Recipient and Kidney Graft Outcomes of Human Immunodeficiency Virus Positive Deceased Donors in the United States
1Division of Nephrology & Hypertension, University of Minnesota, Minneapolis, MN, 2Division of Transplantation, Department of Surgery, University of Minnesota, Minneapolis, MN, 3M-Health Fairview Analytics, Minneapolis, MN
Meeting: 2022 American Transplant Congress
Abstract number: 200
Keywords: Donation, Graft survival, HIV virus, Outcome
Topic: Clinical Science » Kidney » 32 - Kidney Deceased Donor Selection
Session Information
Session Name: Kidney Deceased Donor Selection I
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:50pm-4:00pm
Presentation Time: 3:50pm-4:00pm
Location: Hynes Ballroom C
*Purpose: With the inception of the HIV Organ Policy Act, HIV-positive donor to HIV-positive recipient kidney transplantation is a novel form of transplantation in the United States. Here we compared outcomes of kidney HIV-positive recipients by donor HIV status.
*Methods: Using the Scientific Registry of Transplant Recipients, we identified all primary adult kidney transplant recipients (KTRs) with HIV infection. Recipients were grouped according to the donor HIV status into two groups: HIV R+/D+ (n = 152) and HIV R+/D- (n = 1561). We compared recipients and donor characteristics. The primary outcomes included patient and death-censored graft survival by donor HIV status. Secondary outcomes were delayed graft function (DGF) and the following 1-year outcomes: acute rejection, re-hospitalization, and serum creatinine.
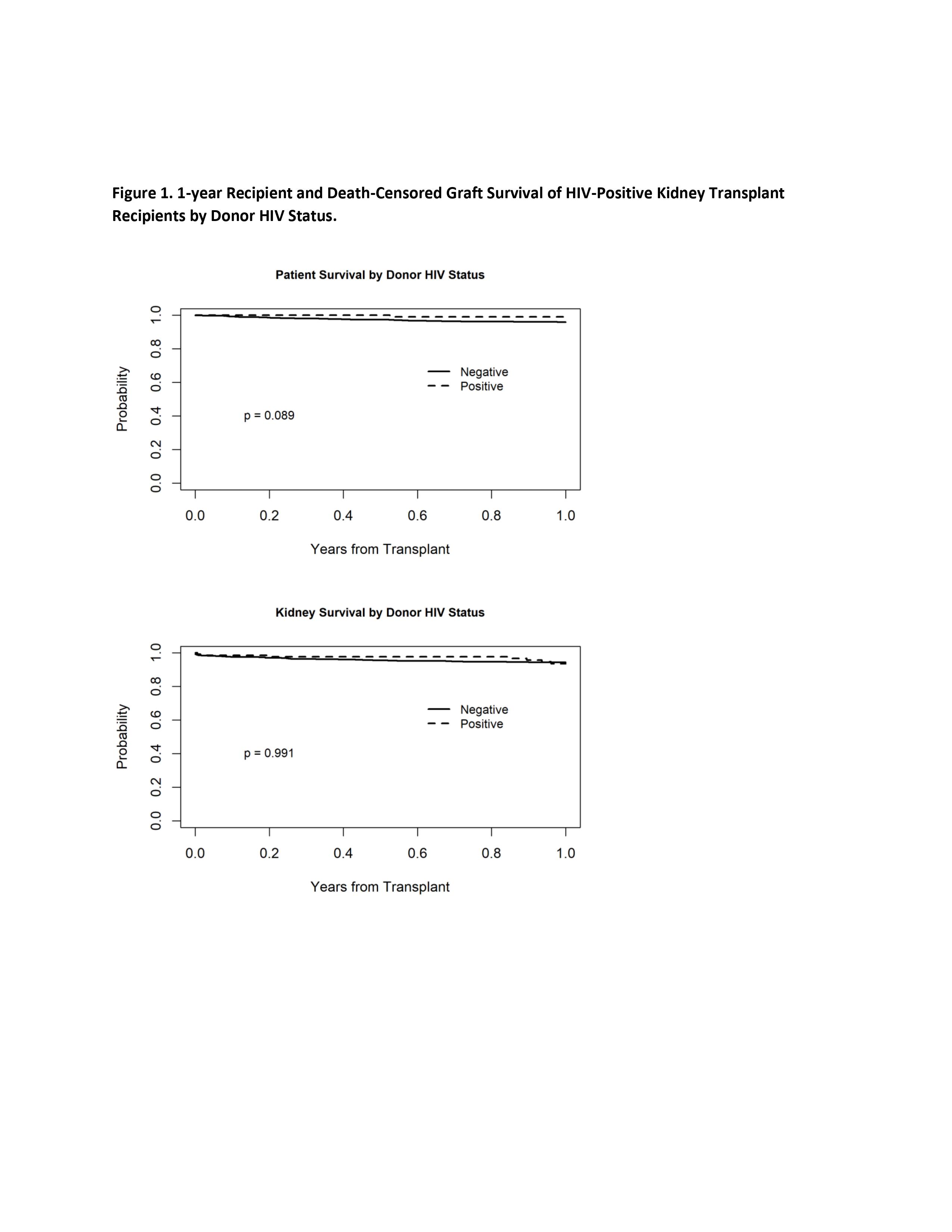
*Results: HIV-positive donors were more likely to be male (73.7% vs. 62.7%, p=0.009), non-white (44.1% vs. 21.0%, p<0.001), and younger (33.50 ± 10.64 years vs. 38.21 ± 15.02 years, p <0.001) compared to HIV-negative donors. In terms of recipient characteristics, HIV R+/D- group had more patients with low (0-20) PRA (73.0% vs 65.1%, p <0.001) and high (80-100) PRA (4.7% vs 0.7%, p <0.001) compared to the HIV R+/D+ group, longer dialysis vintage (7.11 ± 4.16 years vs 4.30 ± 2.38 years, p <0.001), more frequent hepatitis C co-infection (19.3% vs 8.7%, p = 0.002), and steroid-based maintenance immunosuppression (82.0% vs 70.3%, p <0.001). In Kaplan-Meier analysis for survival there was no significant difference in one-year survival between groups (log-rank p=0.089). Similarly, the one-year death censored kidney graft survival was nearly identical (log-rank p= 0.991) (Figure 1). Delayed graft function was less common in the HIV R+/D+ group compared to HIV R+/D- group (23% vs. 38.2%, p <0.001). There were no statistical differences between groups in the one-year outcomes of acute rejection, PTLD or re-hospitalizations.
*Conclusions: Patient and allograft survival for HIV-positive kidney transplant recipients remains comparable between patients who received kidneys from HIV-positive or HIV-negative donors. Using kidneys from HIV-positive deceased donors is a viable option to expand the organ pool for HIV-positive recipients and (perhaps shortens their waiting time). Further research is needed to better elucidate long-term outcomes.
To cite this abstract in AMA style:
Swanson KJ, El-Rifai R, Bregman A, Spong R, Kirchner V, Pruett T, Jackson S, Riad SM. Recipient and Kidney Graft Outcomes of Human Immunodeficiency Virus Positive Deceased Donors in the United States [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/recipient-and-kidney-graft-outcomes-of-human-immunodeficiency-virus-positive-deceased-donors-in-the-united-states/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress