The Role of Geography in Adult Heart Allocation Over the Last 5 Years
1Research, United Network for Organ Sharing, Richmond, VA, 2Mayo Clinic, Rochester, MN, 3Baylor University Medical Center, Dallas, TX
Meeting: 2022 American Transplant Congress
Abstract number: 1125
Keywords: Allocation, Heart
Topic: Clinical Science » Heart » 63 - Heart and VADs: All Topics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: In the last 5 years two policies have impacted the role of geography in adult heart allocation including the 2018 adult heart policy which implemented broader sharing for the most medically urgent candidates and the removal of donor service areas (DSAs) in 2020 . This analysis looks at the impact of both geographic changes on adult heart transplantation.
*Methods: Geographic changes were assessed by comparing cohorts of candidates transplanted pre adult heart implementation (era 1; 10/18/16-10/17/18), post adult heart implementation and pre removal of DSA (era 2; 10/18/18-01/08/20), and post removal of DSA (era 3; 01/09/20-01/08/21) using the OPTN database. Transplants were summarized by era, medical urgency statuses, geography, distance (nautical miles (NM)), and total ischemic time (hours). Equivalent statuses were used for comparisons across eras where old Status 1A was compared to Adult Statuses 1-3, old Status 1B compared to Adult Statuses 4 and 5, and old Status 2 compared to Adult Status 6. Utilization and discard rates were calculated using a cohort of deceased donors by era. Kaplan Meier survival was used to estimate 6-month post-transplant patient survival by era.
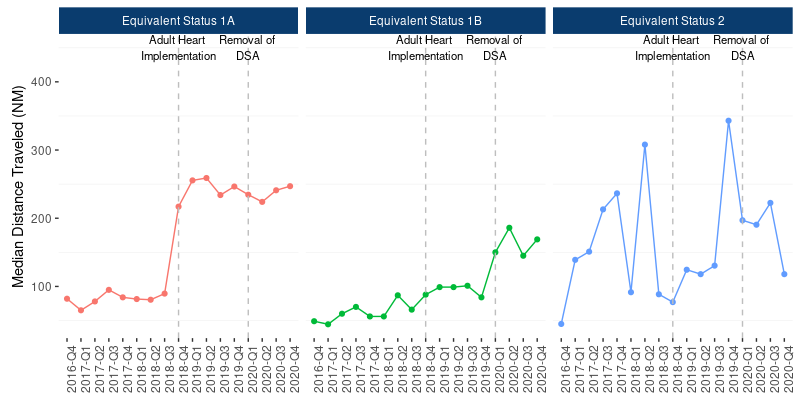
*Results: Transplants continued to increase across all eras. Median distance traveled increased for status 1As (82 vs. 250 NM), status 1Bs (58 vs. 99 NM), and Status 2s (120 vs. 178 NM) from era 1 to era 2. Median distance traveled decreased for Status 1As (250 vs. 235 NM), increased for Status 1Bs (99 vs. 164) and remained the same for Status 2s (178 NM) from era 2 to era 3 (Fig 1). While median distance traveled increased for all statuses from era 1 to era 3, median ischemic times (era 1: 3.1, era 2: 3.4, era 3: 3.4), utilization (era 1: 32.1%, era 2: 30.4%, era 3: 29.7%) and discard rates (era 1: 0.9%, era 2: 0.8%, era 3: 1.0%) remained similar across eras. There were no statistically significant differences between 6-month post-transplant patient survival between the eras (era 1: 93.4%[92.7, 94.1]; era 2: 93.4% [92.6, 94.3]; era 3: 93.2% [92.3, 94.1]).
*Conclusions: Median distance traveled increased following the adult heart policy and the implementation of broader sharing and has since leveled off with the exception of equivalent status 1Bs who have continued to see an increase. Despite increases in distance traveled, ischemic times, utilization and discard rates and post-transplant survival appear to be unaffected. Understanding the effect of distance on organ utilization and outcomes will be important for the transition to continuous distribution.
To cite this abstract in AMA style:
Bradbrook K, Goff R, Daly R, Hall S. The Role of Geography in Adult Heart Allocation Over the Last 5 Years [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/the-role-of-geography-in-adult-heart-allocation-over-the-last-5-years/. Accessed February 23, 2026.« Back to 2022 American Transplant Congress