Impact of a Pharmacist on Transitions and Ambulatory Outcomes in Lung Transplant Recipients
UNC Health, Chapel Hill, NC
Meeting: 2022 American Transplant Congress
Abstract number: 152
Keywords: Graft survival, Osteoporosis, Outpatients
Topic: Clinical Science » Pharmacy » 30 - Non-Organ Specific: Clinical Pharmacy/Transplant Pharmacotherapy
Session Information
Session Name: Non-Organ Specific: Clinical Pharmacy/Transplant Pharmacotherapy
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:00pm-6:10pm
Presentation Time: 6:00pm-6:10pm
Location: Hynes Room 312
*Purpose: Minimal data exists describing the impact of a pharmacist in transitions of care (TOC) and ambulatory medication management in lung transplant recipients (LTRs). Following a 2-tiered implementation of comprehensive pharmacy services, we sought to investigate the impact of a dedicated inpatient and ambulatory lung transplant pharmacy team on both TOC and 1 year clinical outcomes in LTRs.
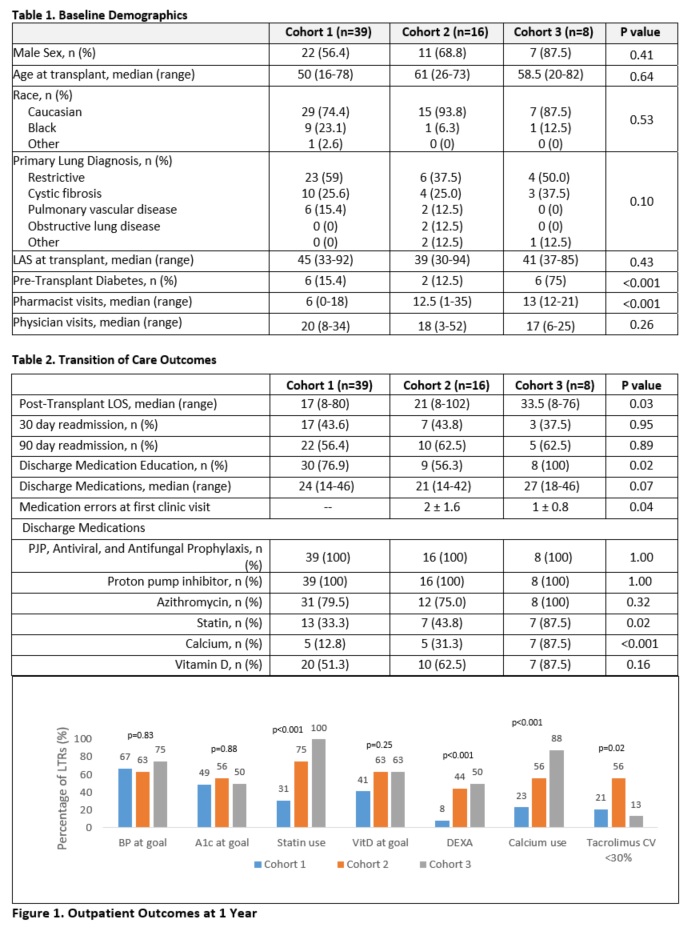
*Methods: A retrospective 3 group cohort study of LTRs was conducted. Cohort 1 included LTRs transplanted from 1/1/2015-12/31/2017 who were seen ad hoc by an ambulatory pharmacist. Cohort 2 included LTRs transplanted from 1/1/2018-12/31/2018 who were seen at each routine ambulatory visit by a pharmacist and physician. Cohort 3 included LTRs transplanted from 1/1/2019-12/31/2019 who were followed inpatient by a dedicated pharmacist then outpatient as per Cohort 2. Dual organ, pediatric and LTRs who did not survive to hospital discharge were excluded. All LTRs received basiliximab induction and tacrolimus, mycophenolate, and prednisone immunosuppression. Outcomes assessed were twofold: TOC outcomes included appropriate guideline-based post-operative anti-infective and preventative medications upon hospital discharge, medication errors at first clinic visit and 30- and 90-day readmissions; ambulatory outcomes included 1 year rates of blood pressure and hemoglobin A1c (A1c) at goal, bone health monitoring and therapies, tacrolimus level variability (assessed by level coefficient of variation [CV]), and appropriate preventative medication regimens. No other protocol changes occurred during the study period. Chi-squared and ANOVA analyses were used.
*Results: 63 LTRs were included, with no significant differences between cohorts other than rate of diabetes at transplant (Table 1). Several TOC outcomes were improved in Cohort 3 compared to Cohort 1 and 2, including increased medication education, reduction in medication errors and increased use of preventative therapies (Table 2). At 1 year, more LTRs in Cohort 2 and 3 were on lipid and bone health therapies, with similar rates of A1c at goal despite a higher rate of underlying diabetes in Cohort 3 (Figure 1). Over 1 year, outpatient pharmacy-led visits significantly increased in Cohort 2 and 3 with no differences in number of physician visits. No differences in rejection or patient/graft survival was seen.
*Conclusions: Based on this single center limited cohort study, integration of dedicated inpatient and ambulatory transplant pharmacists reduced medication errors at index hospital discharge and improved use of supportive care therapies at 1 year post-transplant.
To cite this abstract in AMA style:
Yang A, McKnight R, Prom A, Byrne M, Evans R, Doligalski C. Impact of a Pharmacist on Transitions and Ambulatory Outcomes in Lung Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-a-pharmacist-on-transitions-and-ambulatory-outcomes-in-lung-transplant-recipients/. Accessed January 27, 2026.« Back to 2022 American Transplant Congress