The Gut Microbiome in the Critical Care Setting Post-Heart Transplantation
1Section of Cardiology, University of Chicago, Chicago, IL, 2Duchossois Family Institute, University of Chicago, Chicago, IL
Meeting: 2022 American Transplant Congress
Abstract number: 142
Keywords: Heart, Heart transplant patients, Outcome, Survival
Topic: Clinical Science » Heart » 63 - Heart and VADs: All Topics
Session Information
Session Name: Heart and VADs: All Topics I
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:50pm-6:00pm
Presentation Time: 5:50pm-6:00pm
Location: Hynes Room 210
*Purpose: Given its potential impact on immune activation and systemic inflammation, we aim to investigate gut microbiome compositions and metabolites during critical illness in the immediate post-heart transplant (HT) period.
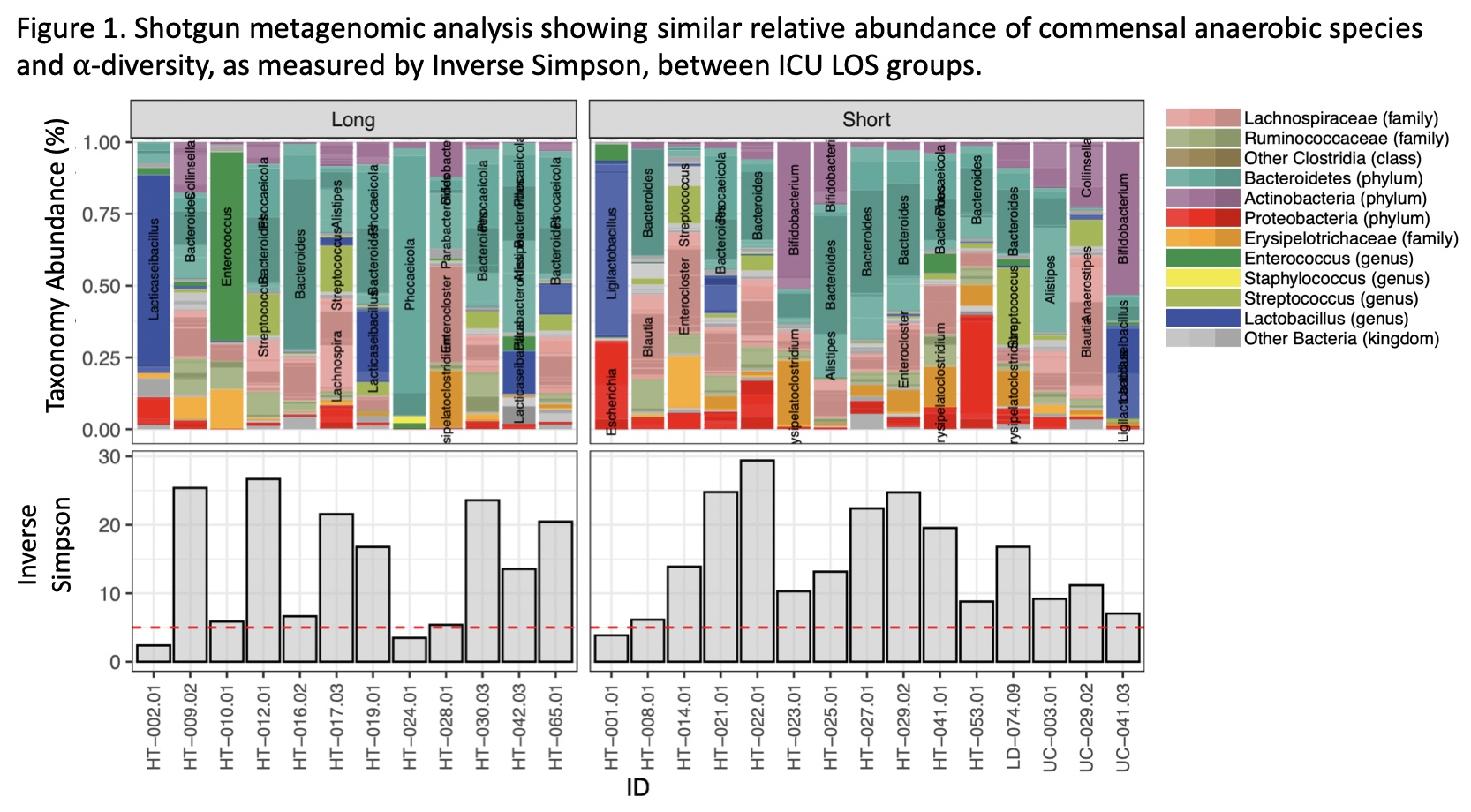
*Methods: We conducted a single-center, cross-sectional study of all HTs performed from July 2020 to August 2021. Stool samples were analyzed for microbiome compositions using shotgun metagenomics and metabolite profiles by mass spectrometry. Subjects were further categorized into groups as defined by: 1.) need for additional pressors; 2.) intensive care unit length of stay (ICU LOS, “short” i.e. less than vs “long” i.e. greater than median); and 3.) duration of vasoactive medication use (“short” i.e. less than or “long” i.e. greater than median duration of inotrope and/or pressor use). Gut microbial diversity, composition, and metabolite production were compared between these groups.
*Results: Twenty-seven HT recipients were included in the analysis. Stool samples were collected a median of 5 days post-HT (IQR [4,9.5] days). Median duration of vasoactive use was 5 days (IQR [4,6] days). Median ICU length of stay was 8 days (IQR [6,12] days). 44% of patients required additional pressors. The groupings based on critical care factors were demographically similar. There was no difference in within-sample microbial or α-diversity between groups. Compositional analysis showed overall similar representation of commensal anaerobic species between the groups as defined by ICU LOS (Fig.1), duration of vasoactive medication use, and additional pressor use. Metabolite analysis revealed similar expression of metabolically active gut microbial products (i.e. short chain fatty acids and secondary bile acids) between groups. Beta-diversity analysis using UMAP did not reveal significant clustering based on any of the critical illness variables.
*Conclusions: In our cohort, HT recipients who needed additional pressors or who experienced higher than average ICU LOS or duration of vasoactive medication use did not exhibit significant differences in gut microbial diversity, composition, or metabolite production compared to patients who did not.
To cite this abstract in AMA style:
Cruz MDela, Lin H, Adler E, Khalid M, Boissiere J, Kim G, Pinney S, Pamer E, Nguyen A. The Gut Microbiome in the Critical Care Setting Post-Heart Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/the-gut-microbiome-in-the-critical-care-setting-post-heart-transplantation/. Accessed March 4, 2026.« Back to 2022 American Transplant Congress