Liver Transplantation in Patients with Portal Vein Thrombosis: Implications and Outcomes
Liver and Pancreas Transplant Center, UCLA, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 124
Keywords: Liver transplantation, Portal veins, Risk factors, Survival
Topic: Clinical Science » Liver » 53 - Liver: Cirrhosis - Portal Hypertension and Other Complications
Session Information
Session Name: Cirrhosis: Complications, Portal Hypertension and Renal Management
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:50pm-6:00pm
Presentation Time: 5:50pm-6:00pm
Location: Hynes Room 311
*Purpose: Preoperative bland portal vein thrombosis (PVT) is common in Liver transplant (LT) candidates and has been suspected to negatively impact post-LT outcomes, however studies in this area remain lacking. We aimed to investigate the impact of pre-LT PVT on outcomes in high acuity recipients.
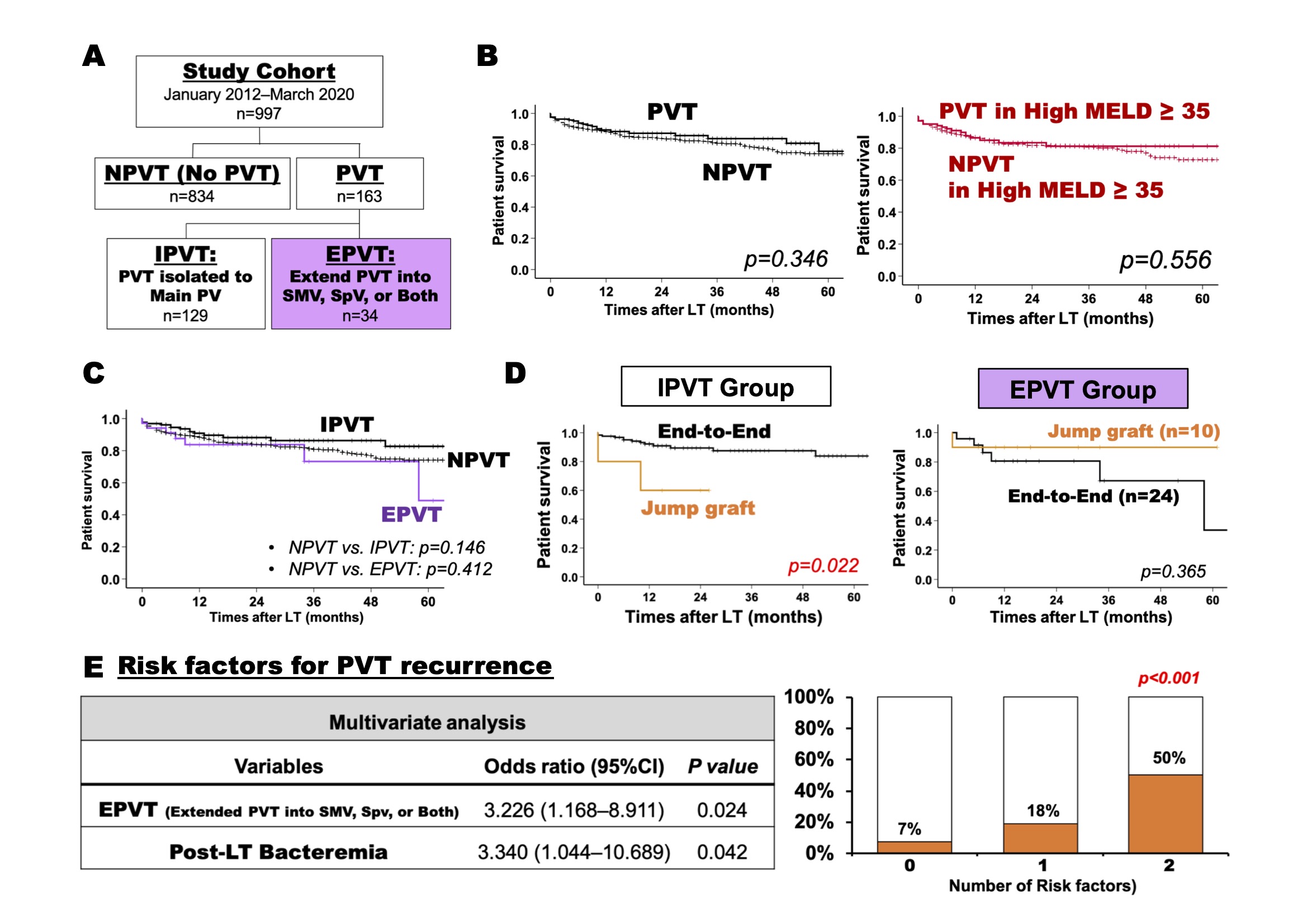
*Methods: Patients with and without preoperative PVT were analyzed. PVT patients were sub-divided into two groups (Fig. A): PVT isolated (IPVT) to the main portal vein vs. Extend PVT (EPVT) into the superior mesenteric vein (SMV), splenic vein (SpV) or both SMV and SpV. Demographics, surgical management and post-LT outcomes including PVT recurrence were compared. Patients with malignant tumors were excluded (Retrospective single center, 997 adult-LT patients, January 2012 to March 2020).
*Results: Of 997 patients, median model for end-stage liver disease (MELD) score was 36, and 163 (16%) had preoperative PVT. Post-LT PVT recurred in 20 patients. PVT and no PVT (NPVT) patients had similar post-LT overall survival rates (Patient p=0.34, Graft p=0.45). In 565 patients with a high MELD score ≥35, there was no significant survival difference between PVT and NPVT (Patient p=0.55, Graft p=0.62; Fig. B). Among all PVT patients, 129 had IPVT, and 34 had EPVT and there were no survival differences between NPVT, IPVT and EPVT patients (Fig. C). During portal reconstruction following thromboendovenectomy, 148 patients received end-to-end anastomosis and 15 required a jump graft. In IPVT, end-to-end anastomosis provided better survival outcomes than jump graft (Patient p=0.02, Graft p=0.04). On the other hand, in EPVT, there were no significant differences between these methods of anastomosis (Fig. D). EPVT (OR 3.22, p=0.02) and post-LT bacteremia (OR 3.34, p=0.04) were detected as significant risk factors for PVT recurrence (Fig. E).
*Conclusions: This is the largest single center series examining the impact of pre-LT PVT on post-LT outcomes. Overall, PVT did not impact post-LT outcomes in high acuity patients. However, the results suggest that extensive PVT not amenable to thromboendovenectomy necessitating a jump graft negatively impacts outcomes. Post LT bacteremia was also identified risk factor for PVT recurrence. These findings may aid in perioperative planning and management.
To cite this abstract in AMA style:
Noguchi D, Rosenthal CJ, Ha M, Agopian VG, Farmer DG, Kaldas FM. Liver Transplantation in Patients with Portal Vein Thrombosis: Implications and Outcomes [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplantation-in-patients-with-portal-vein-thrombosis-implications-and-outcomes/. Accessed March 1, 2026.« Back to 2022 American Transplant Congress