Mortality in Solid Organ Transplant Recipients with a Pretransplant Cancer Diagnosis
1Hennepin Healthcare, University of Minnesota, Minneapolis, MN, 2Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, MD, 3Cancer Registry of Idaho, Boise, ID, 4Epidemiology, University of Iowa, Iowa City, IA, 5North Dakota Statewide Cancer Registry, Grand Forks, ND, 6New Jersey State Cancer Registry, Trenton, NJ, 7Infections and Immunoepidemiology Branch, National Cancer Institute, Bethesda, MD, 8University of South Carolina, Columbia, SC
Meeting: 2022 American Transplant Congress
Abstract number: 63
Keywords: Mortality, Prediction models, Prognosis, Tumor recurrence
Topic: Clinical Science » Organ Inclusive » 67 - Non-PTLD/Malignancies
Session Information
Session Name: PTLD and Malignancies
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:10pm-4:20pm
Presentation Time: 4:10pm-4:20pm
Location: Hynes Room 309
*Purpose: Transplant-associated immunosuppression may cause cancer recurrence in patients with a pretransplant cancer, but little is known about outcomes among these recipients.
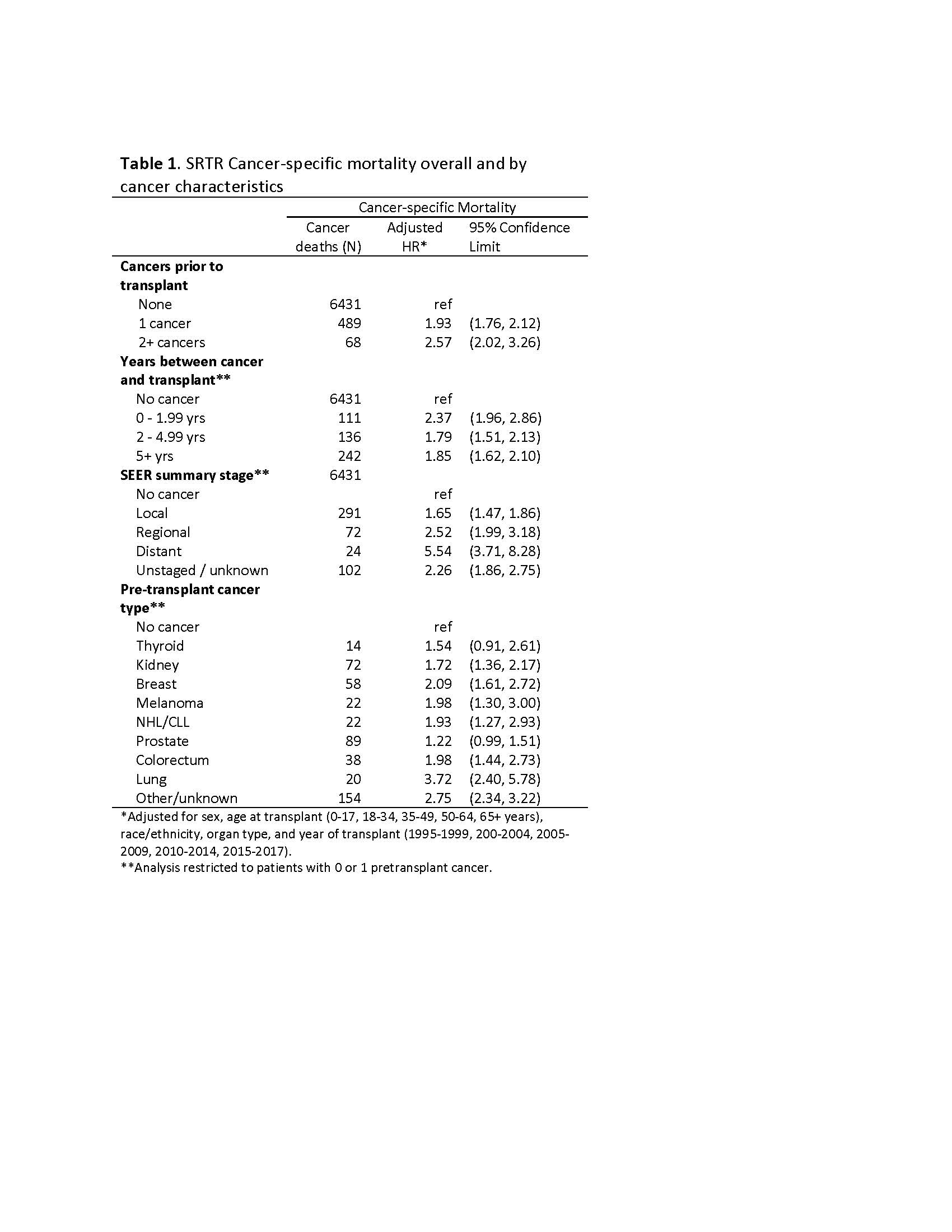
*Methods: We used data from the Transplant Cancer Match (TCM) Study, a linkage of the Scientific Registry of Transplant Recipients (SRTR) with multiple US cancer registries. Cox proportional hazards models assessed the association of pretransplant cancer with overall and cancer-specific mortality, and with risk of a posttransplant de novo (PTDN) cancer, after transplantation. We reviewed cancer registry data on cause of death to determine whether cancer deaths were due to the pretransplant or PTDN cancer.
*Results: Among 311,677 recipients, 11,030 (3.5%) and 1282 (0.4%) had 1 or 2+ pretransplant cancers, respectively. 1 pretransplant cancer was associated with increased overall mortality (adjusted hazard ratio [aHR] 1.19, 95% confidence interval [CI] 1.15-1.23) and cancer-specific mortality (aHR 1.93, 1.76-2.12); results for 2+ cancers were similar. Increased cancer-specific mortality was strongly associated with <2 years between cancer diagnosis and transplantation (aHR 2.37, 1.96-2.86) and distant cancer stage (aHR 5.54, 3.71-8.28). Associations were least strong for thyroid and prostate cancers (aHRs 1.22 and 1.54) and strongest for lung cancer (aHR 3.72). A pretransplant cancer diagnosis was also associated with increased risk of a PTDN (aHR 1.32, 95%CI 1.23-1.40). Among the 307 cancer deaths in patients with a confirmed cancer-specific death in the cancer registry data, 51.6% were due to a PTDN and 34.3% to the pretransplant cancer.
*Conclusions: A pretransplant cancer diagnosis is associated with increased risk of overall and cancer-specific mortality after transplantation, but a substantial fraction of cancer deaths were due to PTDN cancers rather than pretransplant cancer recurrence. Additional studies are needed to determine how the absolute risk increase should be balanced against waitlist mortality. In addition, there is a need to better define recurrence risk and reevaluate posttransplant cancer screening guidelines.
To cite this abstract in AMA style:
Hart A, Pfeiffer R, Morawski B, Lynch C, Zeng Y, Pawlish K, Yu K, Hurley D, Engels E. Mortality in Solid Organ Transplant Recipients with a Pretransplant Cancer Diagnosis [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/mortality-in-solid-organ-transplant-recipients-with-a-pretransplant-cancer-diagnosis/. Accessed February 12, 2026.« Back to 2022 American Transplant Congress