Seroprevalence of HHV8 Among Donors and Recipients with HIV
P. H. Nambiar1, T. Liang2, J. D. Motter3, W. Werbel3, S. Mehta4, V. Kirchner5, M. Rana6, S. Florman7, J. Odim8, W. Miley9, N. Labo9, D. Whitby9, A. Massie10, D. Segev3, A. Tobian3, C. Durand2
1Medicine, Memorial Sloan Kettering Cancer Center, New York, NY, 2Medicine, Johns Hopkins University, Baltimore, MD, 3Johns Hopkins University, Baltimore, MD, 4New York University Langone Transplant Institute, New York, NY, 5University of Minnesota, Minneapolis, MN, 6Icahn School of Medicine at Mount Sinai, New York, NY, 7Mount Sinai Medical Center, New York, NY, 8National Institute of Health, Bethesda, MD, 9National Cancer Institute, Frederick, MD, 10Johns Hopkins School of Medicine, Baltimore, MD
Meeting: 2022 American Transplant Congress
Abstract number: 58
Keywords: HIV virus, Infection, Kidney/liver transplantation, Malignancy
Topic: Clinical Science » Infection Disease » 24 - All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: Cytomegalovirus and other Herpes Viruses
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:50pm-5:00pm
Presentation Time: 4:50pm-5:00pm
Location: Hynes Ballroom B
*Purpose: Kaposi sarcoma (KS) can develop post-transplant via recipient HHV8 reactivation or donor-acquired HHV8. In the general US population, HHV8 seroprevalence is low (1-5%), yet donors and recipients with HIV may have higher HHV8 seroprevalence and increased post-transplant KS risk. Our objective was to understand HHV8 seroprevalence in donors and recipients with HIV.
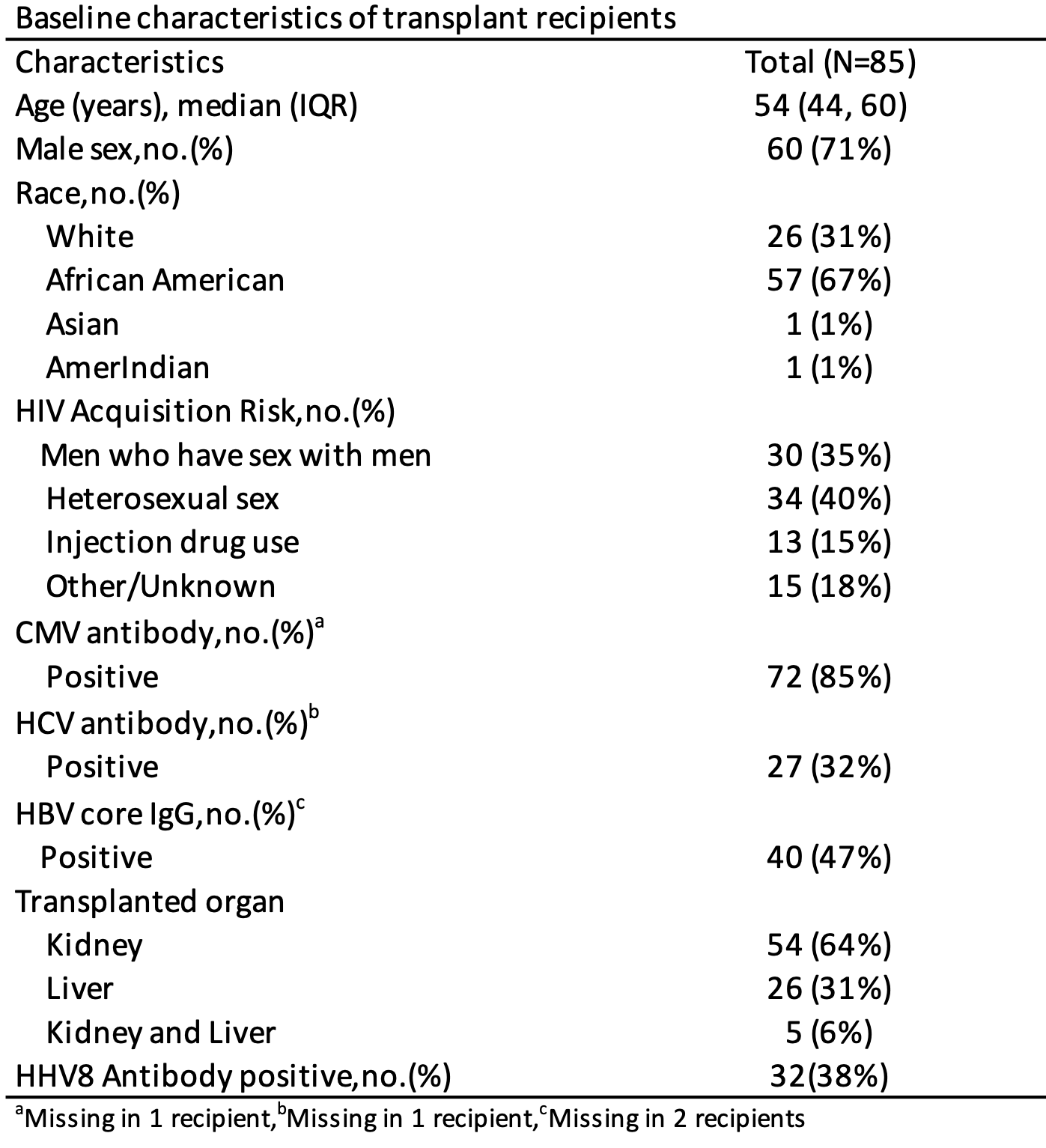
*Methods: Within the HOPE in Action Multicenter study of HIV-to-HIV transplantation, we measured HHV8 seroprevalence in kidney and liver recipients with HIV and in donors with HIV (D+) or false positive HIV tests (FP). Pre-transplant samples were tested for IgG antibodies to HHV8 latent protein ORF73 and lytic protein K8.1 by ELISA; seropositivity was defined as either positive. We compared characteristics of donors by HIV status (D+ vs FP). We performed multivariable logistic regression to identify donor and recipient factors independently associated with HHV8 seropositivity.
*Results: We tested 85 HIV+ recipients (kidney=54, liver=26, simultaneous liver-kidney=5). HHV8 seroprevalence was 38%. HHV8 seropositivity was independently associated with male sex (OR=1.513.6121,p=0.02) and being a man who has sex with men (MSM) (OR=1.34.213.5,p=0.01). We tested 178 donors: 129 D+, 49 FP; HHV8 seroprevalence was 28% and 6%, respectively. Compared to FP, HIV D+ were more likely older (41y vs 34y,p<0.001), CMV positive (78% vs 61%,p<0.001), and HBV core antibody positive (20% vs 0%,p<0.001). Donor HHV8 seropositivity was independently associated with male sex (OR=1.18.973,p=0.04), MSM (OR=1.23.39.1,p=0.02) and HBV core antibody positive (OR=1.53.89.8,p=0.006).
*Conclusions: Within a national study of kidney and liver recipients and donors with HIV, HHV8 seropositivity was substantially higher than has been described in the general population, particularly in males and MSM. HHV8 screening in this population may be warranted to inform post-transplant KS risk and monitoring practices.
To cite this abstract in AMA style:
Nambiar PH, Liang T, Motter JD, Werbel W, Mehta S, Kirchner V, Rana M, Florman S, Odim J, Miley W, Labo N, Whitby D, Massie A, Segev D, Tobian A, Durand C. Seroprevalence of HHV8 Among Donors and Recipients with HIV [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/seroprevalence-of-hhv8-among-donors-and-recipients-with-hiv/. Accessed February 23, 2026.« Back to 2022 American Transplant Congress