Impact of Donor Quality on Outcomes for AKI and Non-AKI Kidneys with and without DGF
1Mayo Clinic Arizona, Phoenix, AZ, 2Division of Transplant Nephrology, Mayo Clinic Arizona, Phoenix, AZ, 3Division of Anatomic Pathology, Mayo Clinic Arizona, Phoenix, AZ
Meeting: 2022 American Transplant Congress
Abstract number: 742
Keywords: Donors, marginal, Graft survival, Kidney transplantation, Organ Selection/Allocation
Topic: Clinical Science » Kidney » 32 - Kidney Deceased Donor Selection
Session Information
Session Name: Kidney Deceased Donor Selection
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: The relevance of DGF, and whether it is clinically significant, continues to be debated. Our aim was to compare post-transplant outcomes between AKI and non-AKI kidneys with and without DGF.
*Methods: We included all deceased donor kidney transplant (KT) recipients at our center between 2008 and 2019. KT from donors with a KDPI>85% were excluded. Donor AKI data was obtained from UNOS DonorNet and was classified using the Acute Kidney Injury Network (AKIN) classification criteria. The study cohort was divided into 2 groups: KT from donors with no or mild AKI (AKIN 0-1), and KT from donors with moderate to severe AKI (AKIN stage 2-3). Our center relies on pre-KT biopsy review for donors with AKIN stage 2-3 AKI, diabetes and hypertension to guide decision-making regarding kidney allograft utilization.
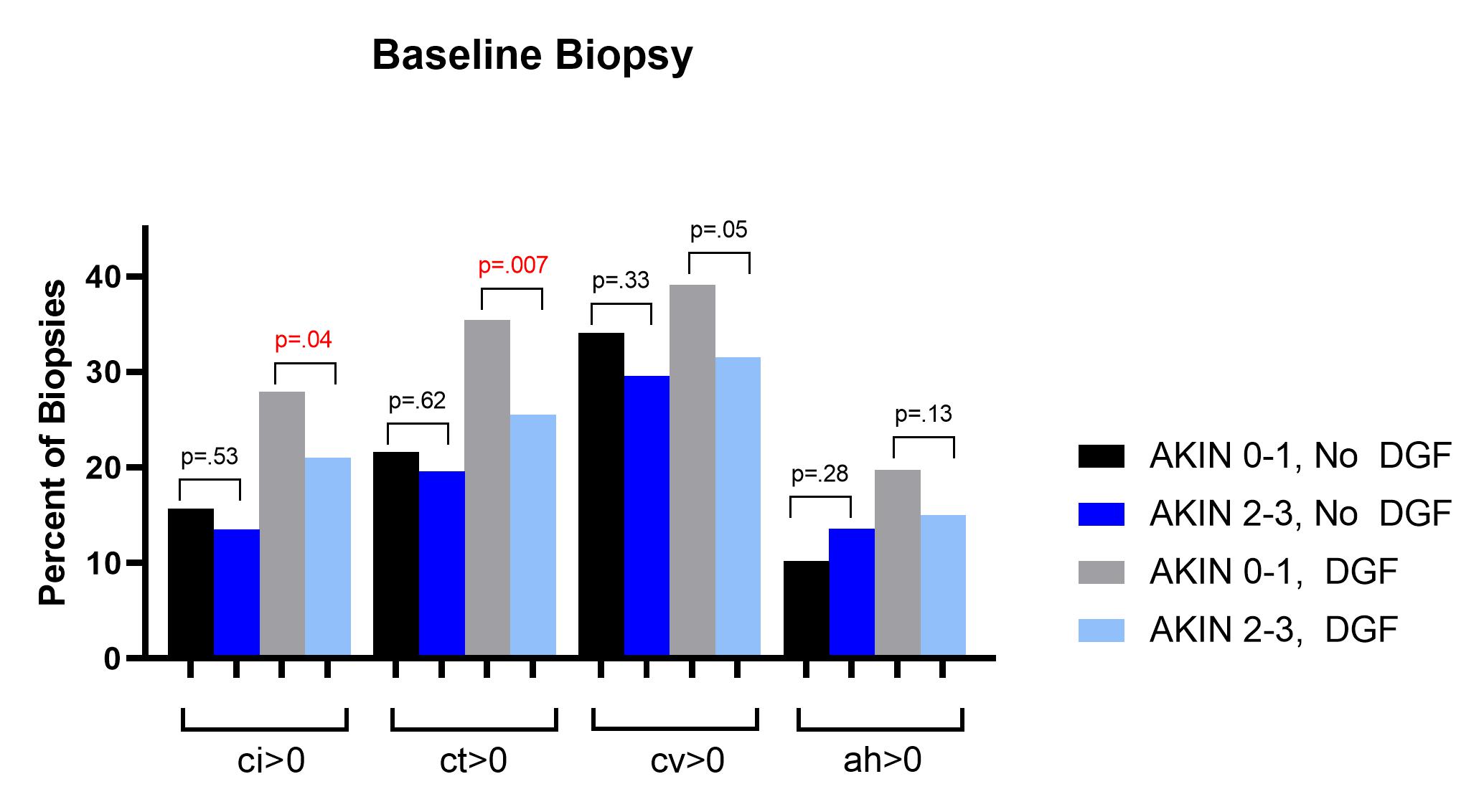
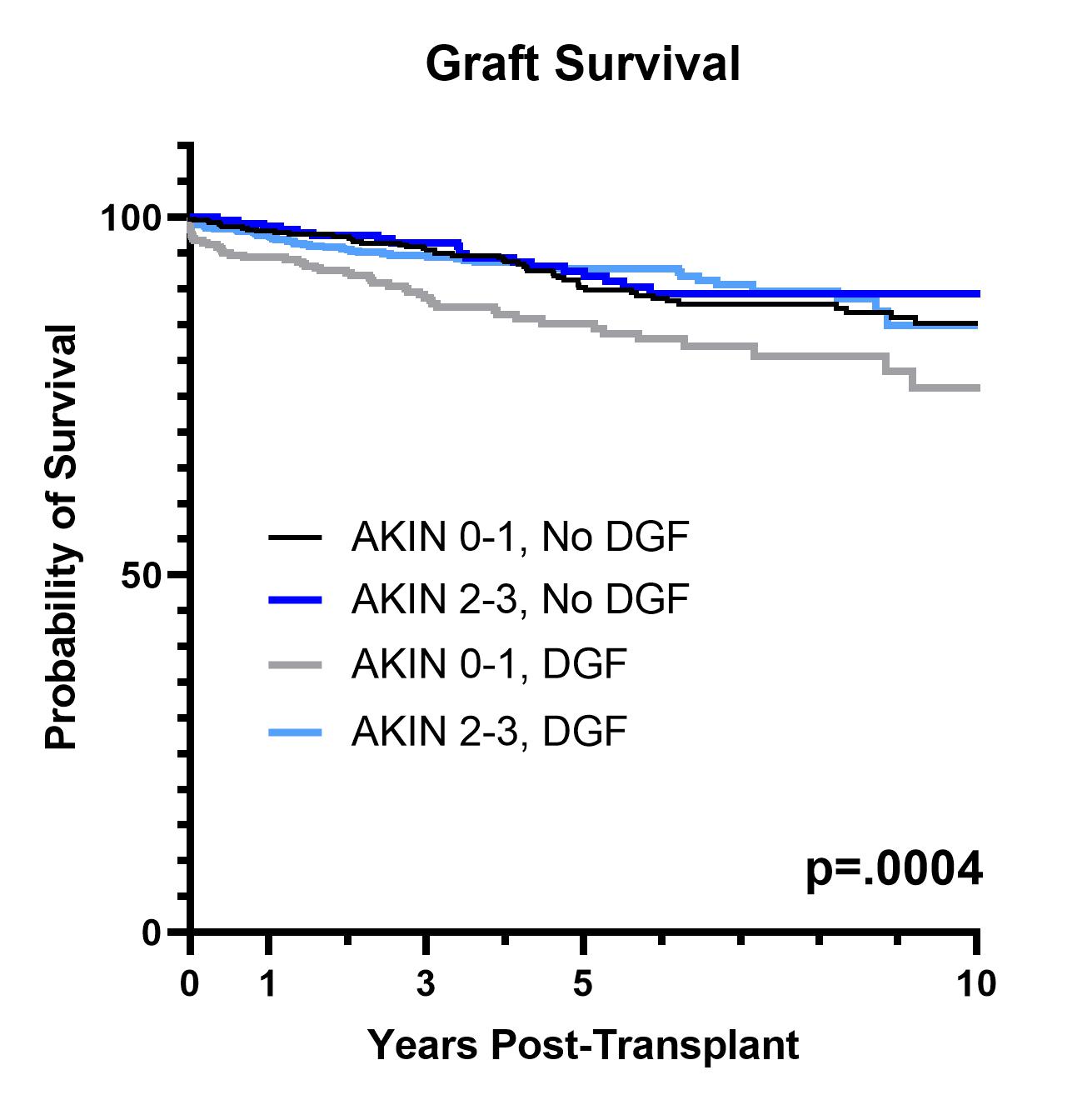
*Results: This cohort included 864 (50.4%) AKIN 0-1 KT and 849 (49.6%) AKIN 2-3 KT. DGF occurred in 39.5% of AKIN 0-1 KT and 71.8% of AKIN 2-3 KT (p<.001). Donors in the AKIN 0-1 group were more likely to be donation after circulatory death (DCD) donors (p<.001) and have died as a result of stroke (p<.001). AKIN 2-3 donors were younger (p=.02), more likely to be male (p<.001), and have longer cold ischemia times. Although there were no differences in KDPI between the AKIN groups (p=.85), baseline KT biopsies showed more chronic changes (ci,ct) in the AKIN 0-1 KT group with DGF (Figure 1). Estimated GFR at 1-year was lower in AKIN 0-1 KT with DGF compared to those without (p<.001); there were no 1-year differences in eGFR for AKIN 2-3 KT with and without DGF (p=.16). Similarly, graft survival was lower for AKIN 0-1 KT with DGF (p<.001) and there were no graft survival differences for AKIN 2-3 KT with and without DGF (p=0.22) (Figure 2). In an adjusted Cox model, the HR was 1.54 (1.12-2.11) in the AKIN 0-1 group and 1.13 (0.77-1.66) in the AKIN 2-3 group.
*Conclusions: The successful use of AKI kidneys relies on careful donor selection. DGF occurs commonly in AKI KT and does not impact graft survival. Baseline donor quality, not DGF itself, plays a significant role in post-transplant outcomes.
To cite this abstract in AMA style:
Jadlowiec C, Budhiraja P, Butterfield R, Smith M, Mathur AK, Moss A, Khamash H, Reddy K, Heilman R. Impact of Donor Quality on Outcomes for AKI and Non-AKI Kidneys with and without DGF [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-donor-quality-on-outcomes-for-aki-and-non-aki-kidneys-with-and-without-dgf/. Accessed March 7, 2026.« Back to 2022 American Transplant Congress