Infections Following Rejection Therapies in Solid Organ Transplant Recipients
S. Gupta1, J. Gea-Banacloche2, H. Me3, D. M. Chascsa4, H. R. Vikram2, R. Yaman1, L. Kodali3
1Internal Medicine, Mayo Clinic, Scottsdale, AZ, 2Infectious Diseases, Mayo Clinic, Phoenix, AZ, 3Transplant Nephrology, Mayo Clinic, Phoenix, AZ, 4Hepatology, Mayo Clinic, Phoenix, AZ
Meeting: 2022 American Transplant Congress
Abstract number: 693
Keywords: Graft failure, Infection, Kidney/liver transplantation, Rejection
Topic: Clinical Science » Infection Disease » 24 - All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: All Infections (Excluding Kidney & Viral Hepatitis) I
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Infections are known complications of solid-organ transplant. They are most prevalent in the first 12 months after transplant when immunosuppression is at its peak. There is a lack of research regarding infections that occur after treatment of transplant rejection. We aim to study patients treated for rejection and understand the differences between those who did and did not develop infections, and thereby understand risk factors for infections.
*Methods: We conducted a retrospective chart review of all liver and kidney transplant recipients treated for rejection at our institution from 2014 to 2020. Only episodes of rejection within 1 year of transplant and infections within 6 months of rejection treatment were included.
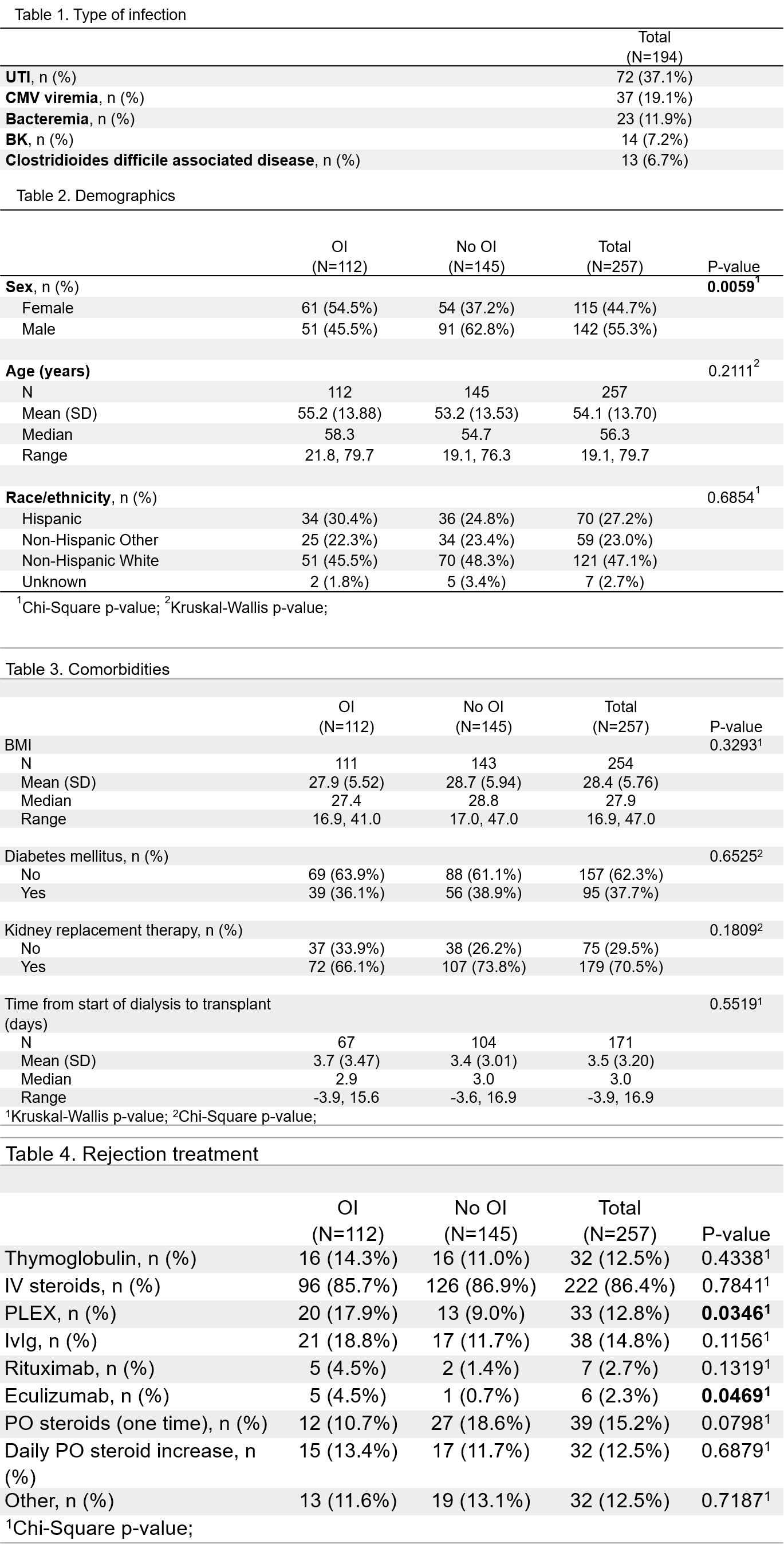
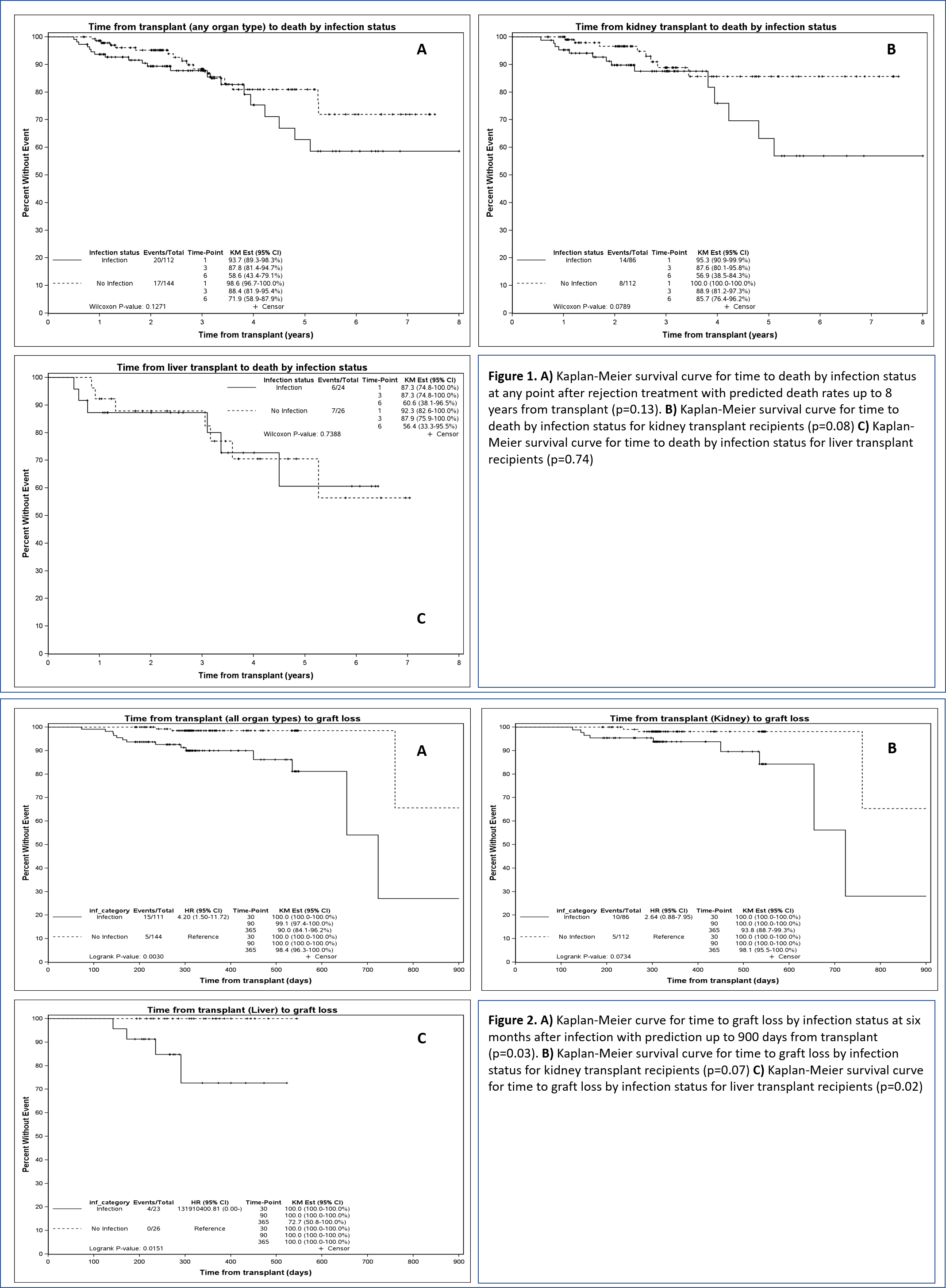
*Results: We identified 257 (199 kidney, 50 liver, 8 simultaneous liver kidney) transplant patients treated for rejection. 112 (43.6%) developed infections and 145 did not. Most common infections are in Table 1. Female gender was found to be a predictor of infection development (p=0.01) (Table 2,3). Eculizumab and plasmapheresis for treatment of rejection were found to be predictors of infections (p=0.04 and 0.05) (Table 4). Outcome data of death at any point and graft loss within 6 months of infection were analyzed and graft loss was found to be significantly associated with infections (p=0.01). Figures 1 and 2 show the association of time to death and graft loss with infections. Though there was no significant difference in patient survival in 2 groups, both allografts had increased failure rates in association with infections.
*Conclusions: Female gender and administration of eculizumab and plasmapheresis for rejection treatment were found to be risk factors for infection. Infections were predictors of graft loss. Though time to death after kidney transplant by infection status was not significant, its p-value indicates that infections may identify a group of patients who are more likely to experience poor outcomes. Further analysis of our data will elucidate relationships between predictors of infection and their associated specific infections.
To cite this abstract in AMA style:
Gupta S, Gea-Banacloche J, Me H, Chascsa DM, Vikram HR, Yaman R, Kodali L. Infections Following Rejection Therapies in Solid Organ Transplant Recipients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/infections-following-rejection-therapies-in-solid-organ-transplant-recipients/. Accessed March 4, 2026.« Back to 2022 American Transplant Congress