Safety and Efficacy of Early Central Line Removal in Post Liver Transplant Patients
1General Surgery, Henry Ford Hospital, Detroit, MI, 2Internal Medicine, Henry Ford Hospital, Detroit, MI, 3Wayne State University School of Medicine, Detroit, MI, 4Henry Ford Transplant Institute, Detroit, MI
Meeting: 2022 American Transplant Congress
Abstract number: 854
Keywords: Infection, Liver transplantation, Outcome, Safety
Topic: Clinical Science » Liver » 51 - Liver: Retransplantation and Other Complications
Session Information
Session Name: Liver: Retransplantation and Other Complications
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Avoiding central line-associated infections (CLABSIs) is paramount in liver transplant recipients. As a hospital-wide infection control initiative at our institution, early removal of central lines after liver transplant (LT) was instituted beginning in September 2019. The aim of the study was to compare the outcomes of patients before and after this change in practice.
*Methods: Retrospective analysis using the databases from a single transplant center and UNOS. 470 adult patients who underwent liver-alone transplants at our institute between January 2017 and June 2021 were included. LTs performed during September 2019 were excluded as a washout period. Demographics, clinical characteristics, and post-transplant outcomes were compared between the pre-and post-policy implementation groups.
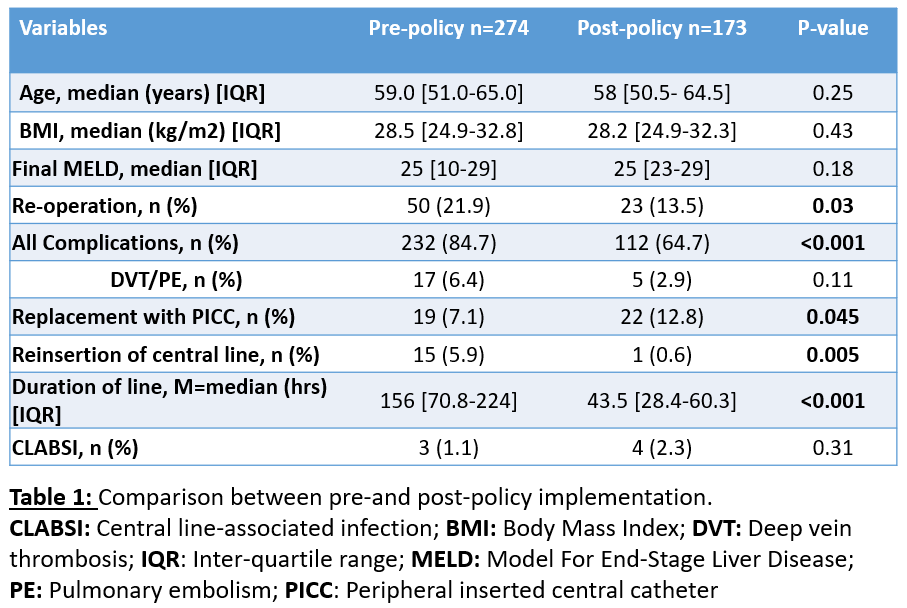
*Results: 447 patients were included in the analysis with 274 patients (61.3%) transplanted prior to the practice change and 173 patients (38.7%) after. Age, gender, race, body mass index, MELD, and etiology of end-stage liver disease (ESLD) did not differ between the 2 groups (Table 1). The median duration of central line placement in the pre-policy period was 156 hours (Interquartile range [IQR]: 71-224) compared to 43.5 hours (IQR: 28.4-60.3) in the post-policy period (p<0.001). 5.9% of pre-policy patients had a central line reinserted during their index post-LT hospitalization compared to 0.6% of post-policy patients (p=0.005). There was a significant increase in the utilization of peripheral inserted central catheter (PICCs) in the index hospitalization post-policy period compared to the pre-policy period (12.8% vs. 7.1%; p=0.045). There was no difference in the rate of CLABSI amongst the two groups (Pre-policy: n=3 [1.1%] vs. post-policy n=4 [2.3%]; p=0.31).
*Conclusions: The early removal of central lines after LT is safe, efficacious, and should be considered in patients without the need for central access. Although CLABSI rates were similar, the shorter central line use was not associated with increased reinsertion of central lines or PICC-associated venous thromboembolism.
To cite this abstract in AMA style:
Shamaa T, MacLean E, Shamaa O, Lu Z, Hinge A, Saymuah S, Mohamed A, Kitajima T, Nagai S, Rizzari M, Yoshida A, Abouljoud M, Collins K. Safety and Efficacy of Early Central Line Removal in Post Liver Transplant Patients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/safety-and-efficacy-of-early-central-line-removal-in-post-liver-transplant-patients/. Accessed January 15, 2026.« Back to 2022 American Transplant Congress