Diffuse Calcification Pattern in Chronic Pancreatitis Has Two Aspects in Total Pancreatectomy with Islet Autotransplantation: Bad Sign for Islet Graft Function and Good Sign for Pain Relief
Baylor University Medical Ctr, Dallas, TX
Meeting: 2021 American Transplant Congress
Abstract number: 1226
Keywords: Islets
Topic: Clinical Science » Pancreas » Pancreas and Islet: All Topics
Session Information
Session Name: Pancreas and Islet: All Topics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Chronic pancreatitis (CP) is characterized by progressive inflammation and fibrosis of the pancreas. The diagnosis of CP is based on pancreatic calcifications, ductal dilatation, and atrophy visualized by imaging with computed tomography (CT) and/or magnetic resonance imaging (MRI). Pancreatic calcification has been previously identified as a major risk factor for development of diabetes in CP patients and poor islet isolation, leading to poor insulin dependence at 1 year after total pancreatectomy with islet autotransplantation (TPIAT). However, the relationship of degree of calcification to TPIAT outcome is not analyzed so far. We retrospectively classified the calcification pattern based on localization, using preoperative CT imaging of CP patients undergoing TPIAT at our center.
*Methods: Our database of 200 consecutive TPIAT procedures performed between 2006 and 2020 was retrospectively reviewed. Based on CT finding, two types of calcification pattern were defined; focal calcification (FC) and diffuse calcification (DC). Glucose level, HbA1c, C-peptide level, daily insulin requirement and insulin independence rate were measured at 3, 6 and 12 months after surgery. Narcotic dose and pain score was also calculated at same time points.
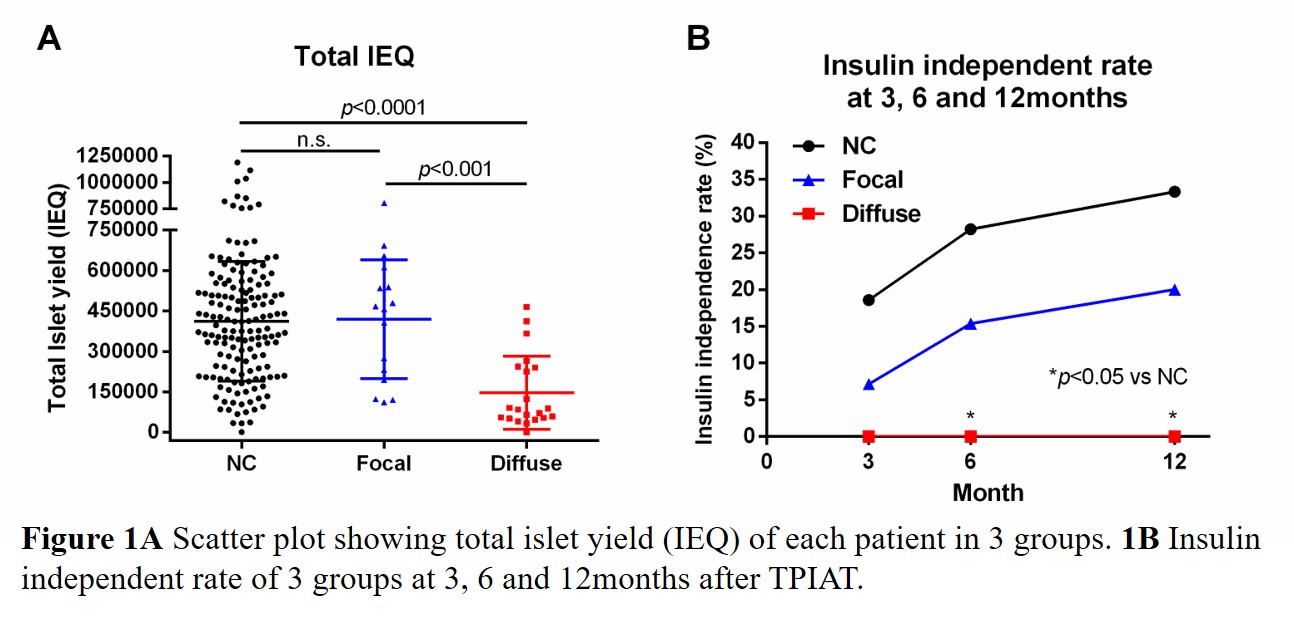
*Results: 37 patients were identified as calcification cases. Among these cases, FC and DC cases were 16 and 21, respectively. Preoperative HbA1c levels of DC group was significantly higher than non-calcification (NC) group (6.5±1.1 vs 5.8±0.9%, p<0.01), and both basal and stimulated C-peptide of DC group were significantly low compared to NC group (basal; 1.2±0.8 vs 1.9±1.2ng/ml, p<0.05, stimulated; 3.2±1.9 vs 6.2±3.5ng/ml, p<0.01). Islet isolation of DC pancreas resulted in lowest total islet yield (IEQ) among the three groups (p<0.0001) and insulin independent rate at 12 month in DC group was 0%. (p<0.05 vs NC) (Figure 1A and B). However, narcotic free rate of DC group at 12 month was 91.7%, significantly higher than other groups (p<0.05 vs FC or NC).
*Conclusions: Simple classification of pancreatic calcification pattern based on CT findings can predict preoperative endocrine function, islet isolation results and metabolic outcomes in CP patients undergoing TPIAT. Although DC is a sign of diabetes risk after TPIAT, DC group also showed advantage on pain relief. These findings suggest TPIAT can provide beneficial effect for patients suffering from severe chronic pancreatitis with calcification.
To cite this abstract in AMA style:
Liu Y, Kumano K, Mattke J, Darden C, Vasu S, Lawrence M, Testa G, Gupta A, Beecherl E, Onaca N, Naziruddin B. Diffuse Calcification Pattern in Chronic Pancreatitis Has Two Aspects in Total Pancreatectomy with Islet Autotransplantation: Bad Sign for Islet Graft Function and Good Sign for Pain Relief [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/diffuse-calcification-pattern-in-chronic-pancreatitis-has-two-aspects-in-total-pancreatectomy-with-islet-autotransplantation-bad-sign-for-islet-graft-function-and-good-sign-for-pain-relief/. Accessed February 23, 2026.« Back to 2021 American Transplant Congress