Healthcare Disparities Amongst Dialysis Patients in North Carolina: Decreased Access to Transplant in Lowest Health Rank Counties
1Cape Fear Valley Medical Center, Fayetteville, NC, 2East Carolina University, Greenville, NC
Meeting: 2021 American Transplant Congress
Abstract number: 1267
Keywords: African-American, Allocation, Economics, Kidney transplantation
Topic: Clinical Science » Organ Inclusive » Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Information
Session Name: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: This study measured healthcare disparities amongst the counties in North Carolina with the best compared with counties with the worst healthcare outcomes, specifically the opportunity for dialysis patients in less healthy counties to receive a kidney transplantation compared to patients in healthier counties.
*Methods: This is a cross-sectional study, utilizing publicly available data from the Health Cost and Utilization Project State Inpatient Database from 2016. Kidney transplant procedures were identified using the diagnosis-related group code 652 and summarized by County. The number patients on dialysis by county was obtained from the North Carolina Division of Health Service Regulation semiannual dialysis report. Utilizing the Robert Wood Johnson Foundation County Health Rankings, we calculated the prevalence of kidney transplantation (KTx) amongst dialysis patients in the top five healthy verses the bottom five unhealthy rank counties. The proportional surgical ratio (PSR), a measure of surgical disparity, was calculated by dividing the observed number of KTx in the 5 lowest rank healthy counties (LRC) by the expected number of KTx using the 5 healthiest counties (HRC) as the standardized reference. Ninety-five percent confidence interval (CI) for the PSR was calculated using Byar approximation.
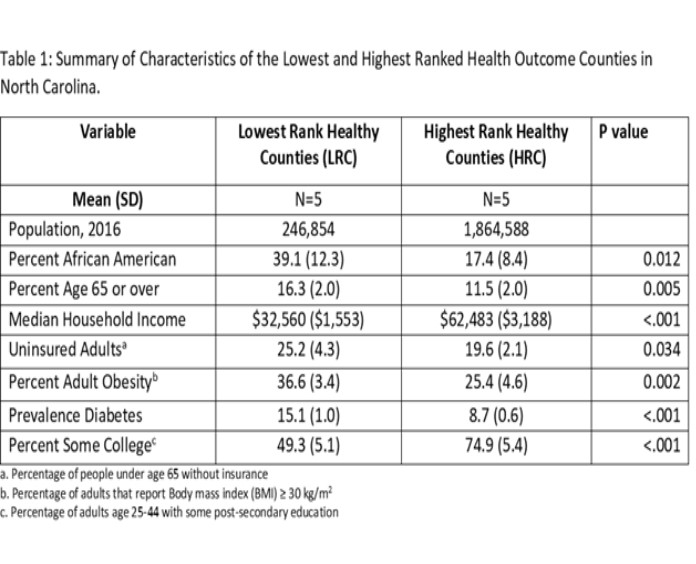
*Results: In 2016 approximately 1.9 million adults lived in the HRC while approximately 246,854 lived in the LRC. Residents in the LRC are typically older, have less education, have lower income, are more likely uninsured and have higher rates of pre-existing conditions compared to residents in the HRC (Table 1). A total of 1,068 individuals in the 5 LRC were on dialysis (4.3 per 1000 population) compared to 3,264 in the 5 HRC (2.1 per 1000 population, p<0.0001). A total of 125 KTx were performed, 19 in the 5 LRC and 106 in the 5 HRC. The rate of KTx in HRC was 32.5 verses 17.9 per 1,000 dialysis-population in the LRC. Using HRC as the reference, the PSR for LRC is 0.55 (95% CI of 0.33, 0.85).
*Conclusions: Within North Carolina, the prevalence of dialysis dependent renal failure is nearly 2.5 times higher in LRC areas while the rate of kidney transplantation is 45% lower.
To cite this abstract in AMA style:
Leto D, Irish W, Haisch C, Tuttle B, Leeser D. Healthcare Disparities Amongst Dialysis Patients in North Carolina: Decreased Access to Transplant in Lowest Health Rank Counties [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/healthcare-disparities-amongst-dialysis-patients-in-north-carolina-decreased-access-to-transplant-in-lowest-health-rank-counties/. Accessed February 21, 2026.« Back to 2021 American Transplant Congress