Pathology of the Explanted Lungs and Surveillance Allograft Biopsy in 202 Lung Transplant Cases: Single Institution Experience
1Pathology, University of Texas Southwestern Medical Center, Dallas, TX, 2Internal Medicine, University of Texas Southwestern Medical Center, Dallas, TX
Meeting: 2021 American Transplant Congress
Abstract number: 1212
Keywords: Lung transplantation, Mortality, Rejection, Survival
Topic: Clinical Science » Lung » Lung: All Topics
Session Information
Session Name: Lung: All Topics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: This study correlates lung transplantation outcomes with pathologic diagnoses of explants and surveillance transbronchial allograft biopsies.
*Methods: A retrospective IRB approved review of archival material from explanted lung recipients from our Department of Pathology database during the period 2013-2016 was performed. Demographic information, explant diagnoses, relevant clinical history, chronology of significant clinical events, and cause of death were retrieved. The results of surveillance allograft biopsies and serum donor specific antigen (DSA) antibodies were also reviewed. Log rank test was used to determine differences in survival among various groups.
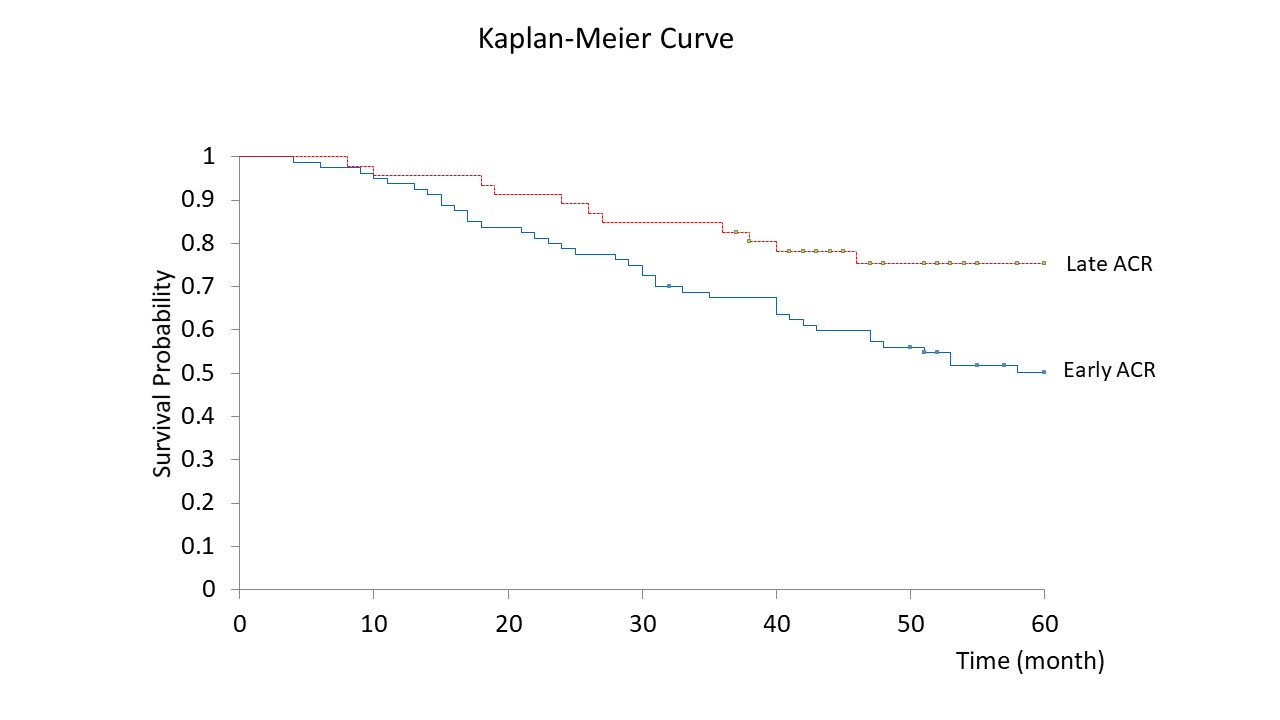
*Results: 202 patients with end-stage lung disease underwent lung transplant during the 4-year study period. The most common explant diagnoses were emphysema (n=63, 31.2%), usual interstitial pneumonia (UIP; n=62, 30.7%), and cystic fibrosis (CF; n=22, 11%). Eighty-eight (43.6%) recipients died during the study period. The most common causes of death were chronic lung allograft dysfunction (n=25, 28.4%), malignancy (n=18, 20.5%), and infection (n=17, 19.3%). Three deaths were related to Coronavirus Disease 2019 (COVID-19). The overall survival rates at 3-year and 5-year were 74.3%, and 62.9%, respectively. Although overall survival rates did not correlate with explant diagnoses, patients with UIP and non-specific interstitial pneumonia (NSIP) tended to have worse outcomes than those with emphysema and CF, with lower survival rates in the first year post-transplant. Allograft rejection was identified in 139 patients (68.8%). Most cases of rejection showed acute cellular rejection (ACR, n=126), while antibody-mediated rejection (AMR) was seen in 29 patients, and a combination of ACR and AMR was found in 15 patients. Patients with early ACR (≤ 90 days post- transplant, n=80) had a lower overall survival rate compared to those with late ACR (> 90 days post-transplant, n=46) with a median survival of 68 vs. 88 months, respectively p<0.05 (Figure 1). In addition, patients with AMR alone tended to have lower survival than patients with both ACR and AMR (median survival 48 vs. 68 months), but not significant (p=0.07).
*Conclusions: This study demonstrates chronic obstructive pulmonary disease (COPD) as the most common indication for lung transplantation in our cohort. Early ACR was associated with adverse outcome by having lower overall survival rate.
To cite this abstract in AMA style:
Sathirareuangchai S, Moore S, Cai Q, Casas LDeLas, Joerns J, Torrealba J. Pathology of the Explanted Lungs and Surveillance Allograft Biopsy in 202 Lung Transplant Cases: Single Institution Experience [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/pathology-of-the-explanted-lungs-and-surveillance-allograft-biopsy-in-202-lung-transplant-cases-single-institution-experience/. Accessed February 16, 2026.« Back to 2021 American Transplant Congress