Role of Recovering Surgeon in DCD Liver Transplant Outcomes
Mayo Clinic, Phoenix, AZ
Meeting: 2021 American Transplant Congress
Abstract number: 1151
Keywords: Donors, non-heart-beating, Liver grafts, Liver transplantation, Outcome
Topic: Clinical Science » Liver » Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Information
Session Name: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Donation after cardiac death (DCD) liver transplant (LT) outcomes have continued to improve. Variability in outcomes has been attributed to center and recovering surgeon experience. The aim of this study was to assess DCD LT outcomes utilizing surgeons from a large volume DCD center versus local recovering surgeons.
*Methods: We assessed 196 DCD LT at our center spanning the years of 2015 to 2020. Multivisceral DCD transplants were excluded.
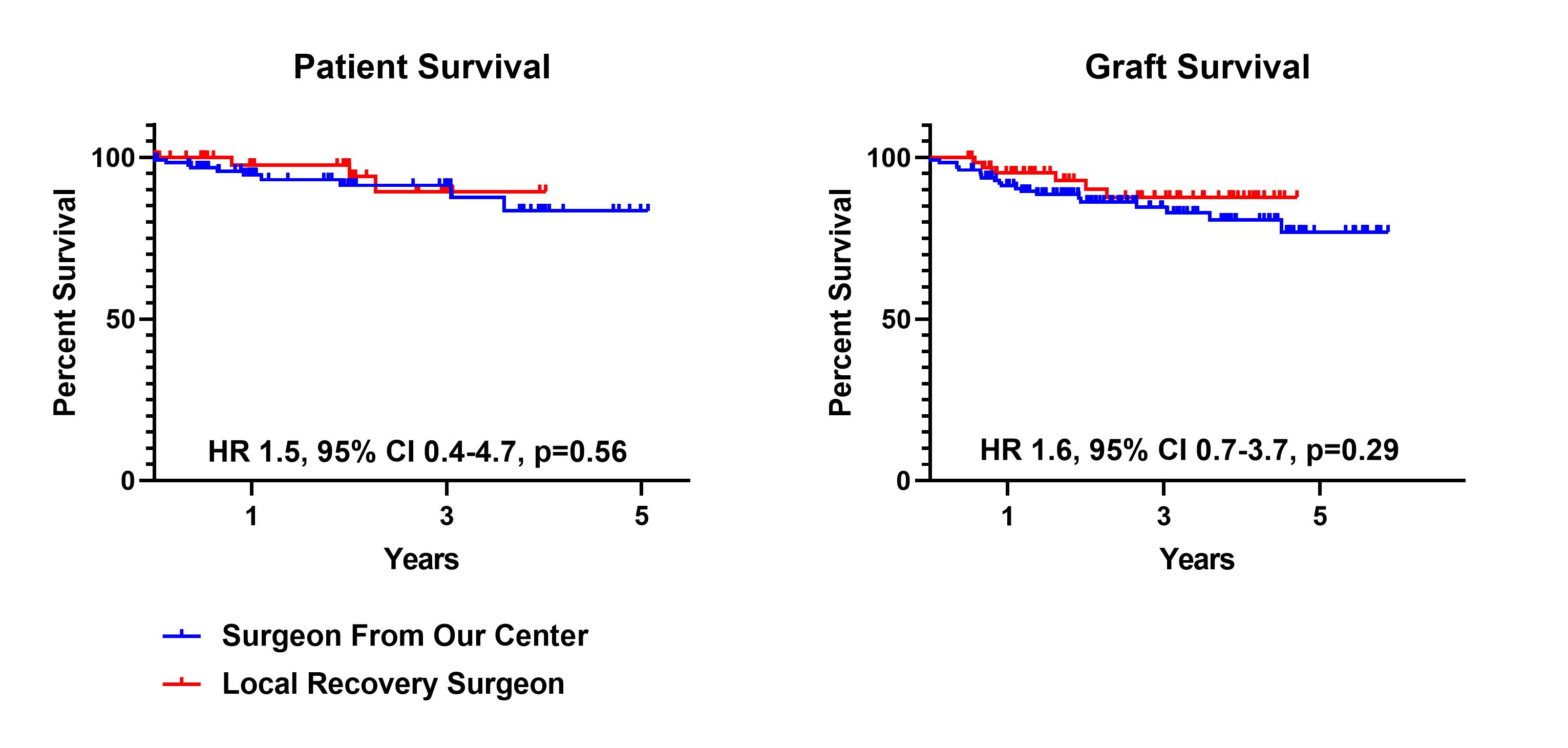
*Results: During this period, there were 129 DCD LT recovered utilizing a surgeon from our center (65.8%) and 67 procured by a local recovery surgeon (34.2%). There were no differences in recipient age (p=0.43) or Model for End Liver Disease (MELD, 20.9±6.0 vs. 20.6±6.2, p=0.77). There likewise were no differences in donor age (p=0.12) and warm ischemia time (WIT) (21.6±6.7 vs. 21.7±4.8, p=0.86). Cold ischemia time was longer for livers recovered utilizing local recovery surgeons (6.4±1.3 vs. 5.2±0.9, p<0.0001). There were no differences in early allograft dysfunction (EAD) (Bili >10, p=0.28; INR >1.6 p=0.70, AST>2000, p=0.33), primary nonfunction rates (0.8% vs. 0.0%, p=0.47) and ischemic cholangiopathy (IC) treated with endoscopy alone (17.1% vs. 11.9%, p=0.35). In total, all-cause IC at any timepoint, including >1 year, requiring re-transplantation was 7.1%. For IC in the absence of hepatic artery (HA) issues, re-transplant rates in the first year were 0.8% for grafts recovered by our center versus 3.0% for those procured by local recovering surgeons (p=0.23). For all-cause IC, including grafts with HA issues, re-LT rates were 3.9% for grafts recovered by our center and 3.0% for those procured by local surgeons (p=0.75). There were no differences in patient (HR 1.5, 95% CI 0.4-4.7, p=0.56) or graft (HR 1.6, 95% CI 0.7-3.7, p=0.29) survival. One-year graft survival for livers recovered by our center was 91.5% compared to 95.5% for grafts with local recovery.
*Conclusions: Excellent DCD LT outcomes can be achieved with the utilization of local recovery surgeons as long as WIT is minimized. Center experience with managing DCD grafts plays a more significant role compared to the role of the recovering surgeon in DCD outcomes. There may be an opportunity to increase utilization of DCD livers by expanding usage of local recovery surgeons.
| Recovery Surgeon From Our Center n=129 | Local Recovery Surgeon n=67 | P value | |
| Hospital LOS, median (days) | 6.0 | 6.0 | 0.71 |
| Day 7 T. Bili >10 (mg/dL) | 5 (3.9%) | 5 (7.5%) | 0.28 |
| Day 7 INR >1.6 (U/L) | 3 (2.3%) | 1 (1.5%) | 0.70 |
| AST >2000 first week | 104 (80.6%) | 50 (74.6%) | 0.33 |
| PNF | 1 (0.8%) | 0 (0.0%) | 0.47 |
| Cholangiopathy requiring endoscopy | 22 (17.1%) | 8 (11.9%) | 0.35 |
| All-cause cholangiopathy requiring re-LT within 1 year | 5 (3.9%) | 2 (3.0%) | 0.75 |
To cite this abstract in AMA style:
Macdonough E, Pont K, Aqel B, Valenti K, Hewitt W, Moss A, Reddy KS, Jadlowiec C. Role of Recovering Surgeon in DCD Liver Transplant Outcomes [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/role-of-recovering-surgeon-in-dcd-liver-transplant-outcomes/. Accessed February 16, 2026.« Back to 2021 American Transplant Congress