Outcomes of DCD Allografts in Liver Transplant Recipients with HCC
1School of Medicine, Mayo Clinic Arizona, Phoenix, AZ, 2Hepatology, Mayo Clinic Arizona, Phoenix, AZ, 3Biostatistics, Mayo Clinic Arizona, Phoenix, AZ, 4Transplant Surgery, Mayo Clinic Arizona, Phoenix, AZ
Meeting: 2021 American Transplant Congress
Abstract number: 1145
Keywords: Donors, non-heart-beating, Hepatocellular carcinoma, Liver transplantation
Topic: Clinical Science » Liver » Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Information
Session Name: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Early studies demonstrated inferior survival for liver transplant (LT) recipients with hepatocellular carcinoma (HCC) who received allografts from donation after cardiac death (DCD) donors vs donation after brain death (DBD) donors. DCD livers have been proposed as a way to decrease waiting time to transplantation. However, prior studies demonstrated increased risk of recurrence with shorter waiting times. The purpose of this study was to examine the impact of using DCD grafts on transplant waiting time, and graft and patient survival for recipients with HCC when compared to DBD recipients.
*Methods: Retrospective review was conducted on all patients who underwent LT for HCC at our institution from 2014 to 2019. Exclusion criteria were: living donor transplants, re-transplants, and incidental HCC diagnosis on explant. Data was collected on recipient and donor demographics, transplant and donor characteristics, tumor characteristics, and patient and graft outcomes. Survival analyses were conducted on HCC recurrence, graft failure, and death using Cox regression models and Kaplan Meier curves.
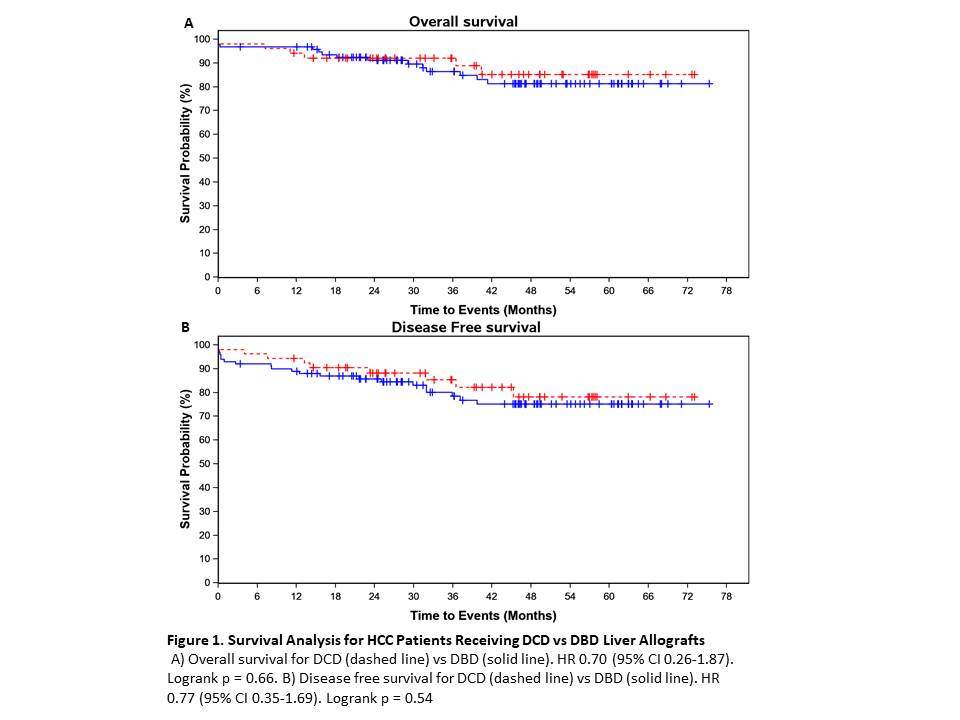
*Results: 153 patients underwent LT: 53 received a DCD organ and 100 received a DBD organ. The median transplant MELD for DCD recipients was 24.0, and for DBD recipients was 25.0 (p=0.99). 66% of DCD recipients received exception points, while 58% DBD recipients had exception points (p=0.39). There was no significant difference in AFP or tumor stage at diagnosis for DCD vs DBD recipients. The mean time from listing to transplant for DCD recipients was 7.2 months vs 5.8 months for DBD recipients (p=0.02). The HCC recurrence rate in DCD recipients was 5.7% vs 9.0% in DBD recipients (p=0.54). Multivariate analysis did not show a difference in overall (HR 1.40 (CI 0.52, 3.79) p=0.506) or disease free survival (HR 1.72 (CI 0.74, 4.00) p=0.207) for patients who received exception points. Overall and disease free survival was similar for patients who received DCD vs DBD allografts (Figure 1).
*Conclusions: Overall patient survival and disease free survival was not affected by the use of DCD grafts. MELD exception at time of transplant was not associated with a higher likelihood of receiving a DBD graft. Transplant waiting time was longer in recipients of DCD grafts, though overall transplant waiting time and MELD score at transplant were low, reflecting the aggressive donor selection approach at our institution.
To cite this abstract in AMA style:
Gupta N, Daum J, Aqel B, Mi L, Harbell J. Outcomes of DCD Allografts in Liver Transplant Recipients with HCC [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-dcd-allografts-in-liver-transplant-recipients-with-hcc/. Accessed February 10, 2026.« Back to 2021 American Transplant Congress