Early Conversion to Belatacept-based Therapy Improves Graft Function in Renal Transplant Patients
1Surgery, SUNY Upstate Medical University, Syracuse, NY, 2Pharmacy, SUNY Upstate Medical University, Syracuse, NY, 3Pathology, SUNY Upstate Medical University, Syracuse, NY, 4Medicine, SUNY Upstate Medical University, Syracuse, NY
Meeting: 2021 American Transplant Congress
Abstract number: 935
Keywords: Graft function, Immunosuppression, Kidney transplantation, Outcome
Topic: Clinical Science » Kidney » Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Information
Session Name: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Our goal in this study was to assess the impact of early vs late conversion to Belatacept based (Bela) IS in kidney transplant (KT) recipients
*Methods: We collected data on renal transplant recipients from 2016-2020 that were converted to a Belatacept-based IS regimen. Patients were stratified into an early-converted group if starting Bela therapy within 26 weeks of transplantation and late-conversion group if treatment was initiated after 26 weeks. Primary outcomes assessed graft function with estimate glomerular filtration rate (GFR). Secondary outcomes included serum creatinine (sCr) and glucose levels
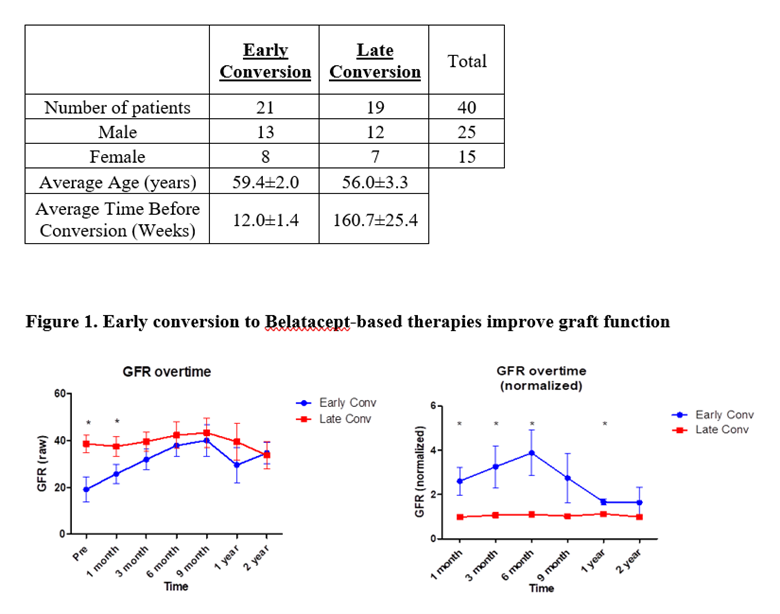
*Results: At our institute total 40 patients converted to Belatacept based IS (Image 1). Early conversion to Bela-therapy significantly enhanced graft function as measured by GFR. Early conversions had a significant increase in GFR from 19±5.3 mL/min to 40.0±6.8 mL/min by the ninth month (p=0.015) and 34.6±4.6 mL/min by the two-year mark (p=0.023). The late conversions had a higher baseline GFR of 38.6±3.8 that was saw little to no deviation over the two years ranging between 33 and 43 mL/min. (Image 1). Before conversion to Bela, average serum creatinine (sCr) was 3.12 (±0.38) and 2.06 (±0.17, p=0.0017) in the early and late groups, respectively. After conversion, the early group experienced a 33% decrease in sCr by the 2-year mark (p=0.0017) compared to their baseline values. Conversely, the late-converted group did not have significant deviations from respective baseline values prior to conversions. At 1, 6, and 24 months post-conversion, the early converted group saw significant improvements in sCr compared to the late converted group with sCr levels decreasing by 13% (p=0.04), 23% (p=0.015), and 38% (p=0.011), respectively.
There was no statistical significance between early and late conversion groups on metabolic glucose levels. There was no significant difference in the number of acute rejections between the two groups (early – 6 events or 29%, late – 5 events or 26%)
*Conclusions: Our study has shown that early Belatacept conversion improves kidney graft function more effectively than later conversion. Therefore, early conversion to Belatacept based IS therapy may be considered more often in selected patients after kidney transplantation
To cite this abstract in AMA style:
Huang N, Yang CJ, Movileanu I, Dvorai RH, Ecal KM, Saidi RF, Senay ANAyla, Gallay B, Hanlon MJ, Narsipur S, Laftavi MR, Shahbazov R. Early Conversion to Belatacept-based Therapy Improves Graft Function in Renal Transplant Patients [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/early-conversion-to-belatacept-based-therapy-improves-graft-function-in-renal-transplant-patients/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress