Cardiac Risk Assessment in Liver Transplant Candidates: Survey of National Practice Patterns
1Div. of GI/Hepatology, University of California, San Diego, San Diego, CA, 2Anesthesiology, Mayo Clinic, Jacksonville, FL, 3Div. of GI/Hepatology, Northwestern University, Chicago, IL
Meeting: 2021 American Transplant Congress
Abstract number: 246
Keywords: Liver transplantation, Screening
Topic: Clinical Science » Liver » Liver: Recipient Selection
Session Information
Session Name: Liver Recipient Selection
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 7, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:55pm-5:00pm
Presentation Time: 4:55pm-5:00pm
Location: Virtual
*Purpose: Cardiac disease is a leading cause of morbidity and mortality in the first year after liver transplantation (LT) and pre-transplant identification is vital to post-transplant outcomes. However, clear evidence-based practice guidance for cardiac risk assessment in LT candidates is lacking. We sought to characterize current practice patterns across transplant centers.
*Methods: We surveyed 117 LT programs across the United States using Research Electronic Database Capture (REDCap). The survey addressed personnel involved, protocols utilized, and specific modalities used in risk assessment and diagnosis of coronary artery disease (CAD) and cardiac function.
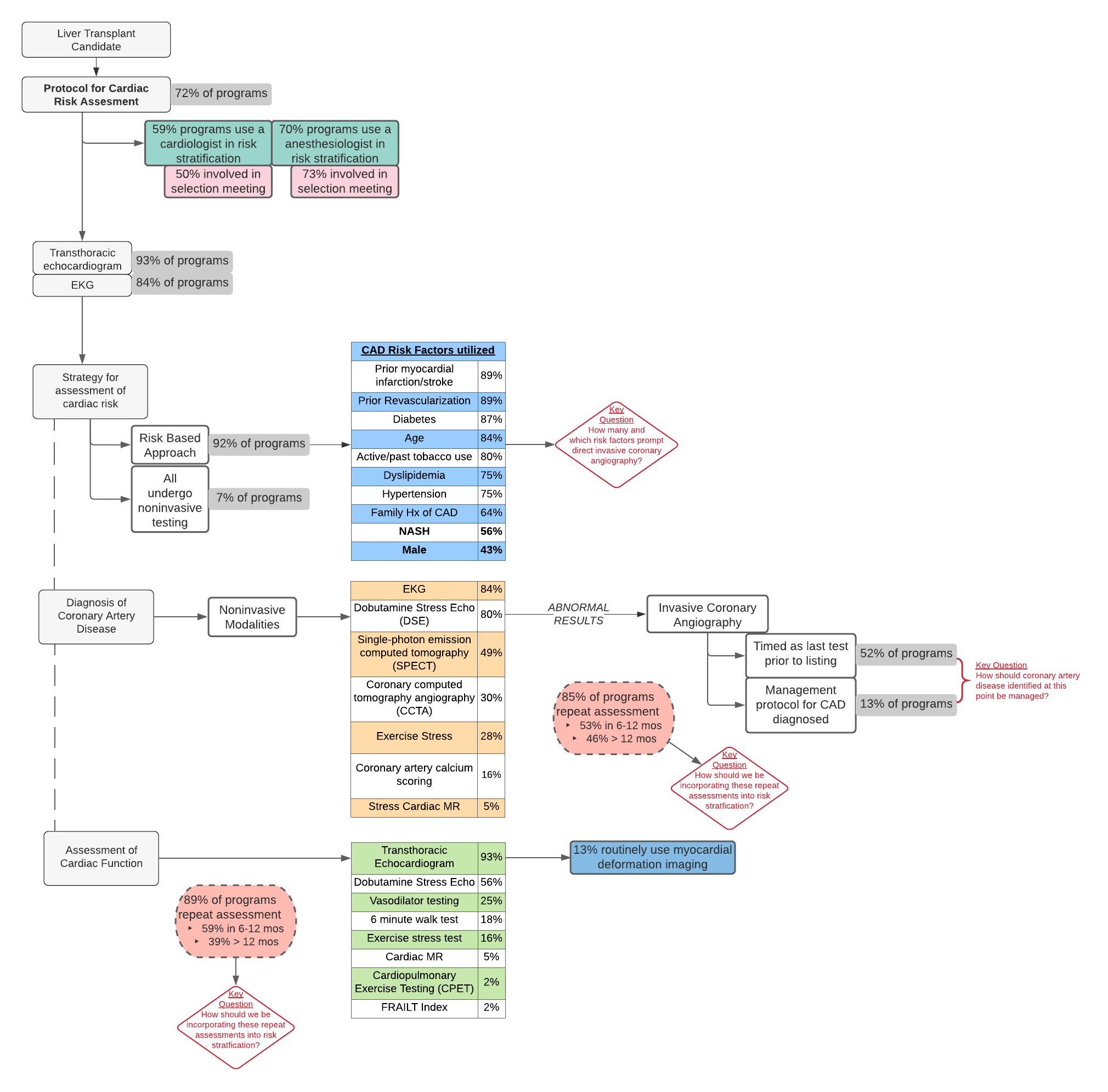
*Results: Of 61 responses, the majority (72%) of programs had a written protocol for risk assessment. 36 programs utilized a dedicated cardiologist for risk stratification, and 50% were involved in selection meeting. Most (70%) programs involved an anesthesiologist in risk stratification; 73% of these were involved in selection meeting. For assessment of cardiac risk, 92% of programs utilized a risk-based approach. The most commonly used risk factors were prior MI/stroke (89%), revascularization (89%), diabetes (87%), age (84%), and smoking (80%); only 56% used NASH as a risk factor. The age threshold to trigger additional testing ranged from 30-70 years old with caveats based on specific risk factors. For non-invasive testing in CAD, most programs used EKG (84%) and dobutamine stress echocardiography (80%). Less than half (49%) used single-photon emission computed tomography and only 30% routinely used coronary computed tomography angiography. Over half (52%) deferred invasive coronary angiography as the last test prior to listing, however only 8 (13%) programs had a specific protocol for management of identified CAD. For cardiac function, nearly all programs (93%) obtained an echocardiogram, though only 8 (13%) programs routinely utilized myocardial deformation imaging; 56% specifically used DSE for this indication. Finally, most programs repeated assessment for both CAD and cardiac function (85% and 89%, respectively) though time interval varied from < 6 months to > 2 years.
*Conclusions: Practice patterns for cardiac risk assessment in LT candidates are heterogeneous across the country and do not reflect current evidence-based recommendations (Figure). This represents an area ripe for standardization to improve identification of cardiac disease and optimize risk for cardiac events after transplant.
To cite this abstract in AMA style:
Barman P, Chadha R, VanWagner L. Cardiac Risk Assessment in Liver Transplant Candidates: Survey of National Practice Patterns [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/cardiac-risk-assessment-in-liver-transplant-candidates-survey-of-national-practice-patterns/. Accessed February 14, 2026.« Back to 2021 American Transplant Congress