Liver Simulated Allocation Model Does Not Accurately Predict Organ Offer Decisions in Pediatric Liver Transplant Candidates
1US Naval Academy, Annapolis, MD, 2Johns Hopkins, Baltimore, MD, 3Univ of Washington, Seattle, WA, 4UCSF, San Francisco, CA, 5Univ of Pittsburgh, Pittsburgh, PA
Meeting: 2021 American Transplant Congress
Abstract number: 414
Keywords: Allocation, Liver transplantation, Pediatric, Prediction models
Topic: Clinical Science » Public Policy » Non-Organ Specific: Public Policy & Allocation
Session Information
Session Name: Adherence, Economics, and Ethics
Session Type: Poster Video Chat
Date: Sunday, June 6, 2021
Session Time: 7:30pm-8:30pm
 Presentation Time: 7:40pm-7:50pm
Presentation Time: 7:40pm-7:50pm
Location: Virtual
*Purpose: The U.S. relies on the Scientific Registry of Transplant Recipient’s (SRTR’s) Liver Simulated Allocation Model (LSAM) to predict the effect of allocation policy changes on liver transplant (LT) outcomes. To effectively inform policy changes, LSAM’s model must accurately predict liver offer accept/decline decisions for candidates in general–and for vulnerable subgroups in particular. We hypothesized that liver offer decisions for children differ fundamentally from adults, and thus that LSAM may not accurately model accept/decline decisions for children.
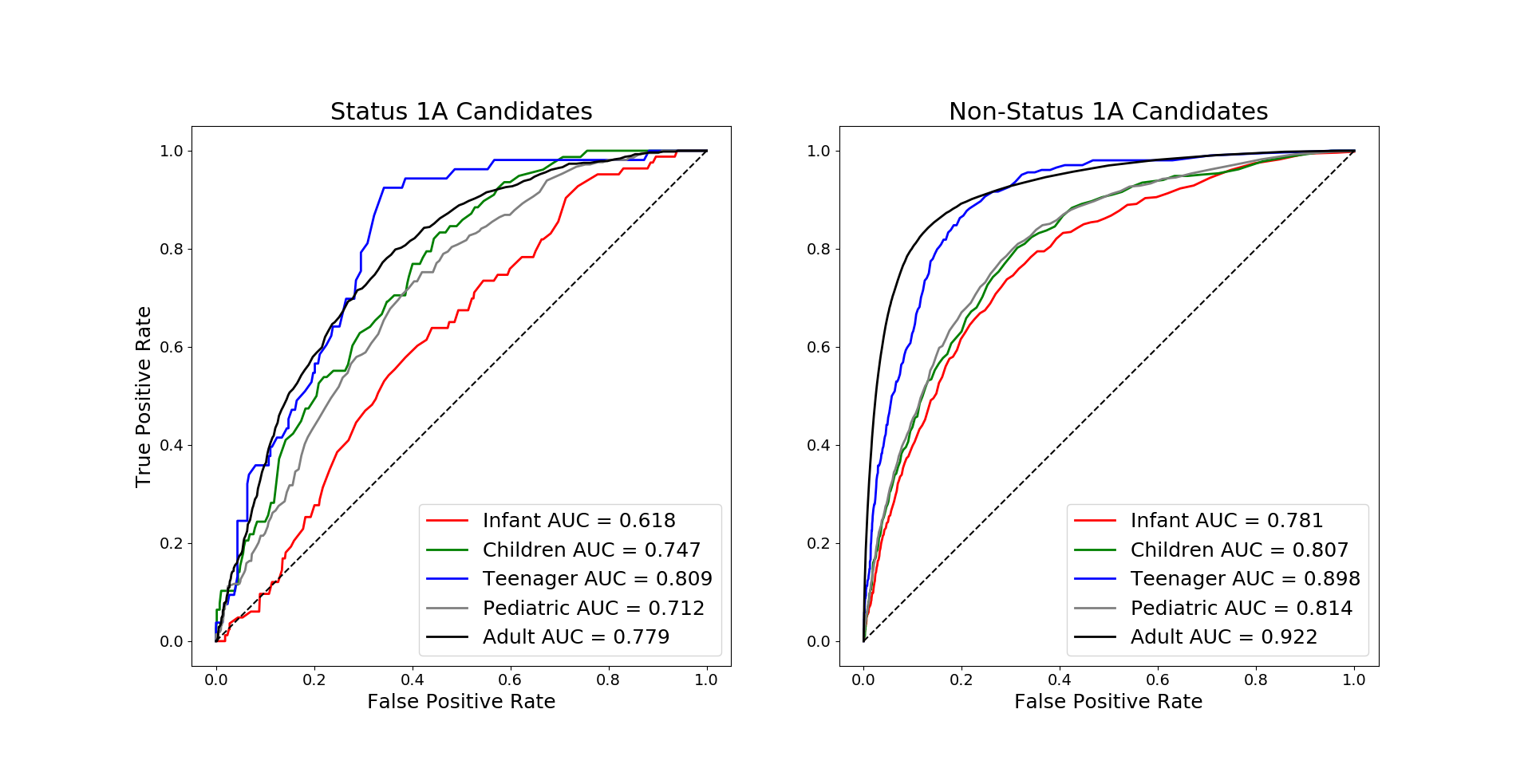
*Methods: SRTR data on all deceased donor liver offers from 07/01/2013-06/30/2016 were compared to LSAM’s model predictions on accept/decline decisions for these LT candidates, to evaluate LSAM predictions in pediatric (listing age <18yrs) vs. adult candidates (≥18yrs). 0.5% of all offers excluded for missing data. Performance of LSAM’s two models, for Status 1A candidates and for non-1A candidates, was evaluated by age group using area under the receiver operator characteristic curves (AUC).
*Results: Of 39,351 offers to pediatric candidates and 894,221 to adults during the analysis period, 95.4% and 99.6% respectively were to non-1A candidates; 2.9% of these offers to children and 1.8% of offers to adults were accepted for LT. Among Status 1A candidates (1,829 children, 3,833 adults), 11.7% and 14.8% of offers were accepted respectively. Among non-1A candidates, LSAM’s prediction of waitlist mortality was substantially worse for pediatric candidates than for adults (AUC 0.814, 0.922 respectively, FIGURE). Stratifying children by age demonstrates that LSAM performed comparably for teenagers (12-17yrs, AUC 0.922) and adults (≥18yrs, AUC 0.898) but much worse for children (2-11yrs, AUC 0.807) and infants (<2yrs, AUC 0.781). For the smaller group of Status 1A candidates, AUC was lower for all age groups but again the lowest for infants (0.618), followed by children (0.747); AUC for teenagers (0.712) was comparable to that of adults (0.779).
*Conclusions: LSAM does not accurately predict liver offer accept/decline decisions for pediatric liver transplant candidates. Predictions are least accurate for the youngest children. To truly predict the impact of allocation policy changes on children, for liver and all solid organ transplants, SAM models specific to pediatrics should be derived and utilized.
To cite this abstract in AMA style:
Wood NL, Mogul DB, Hsu EK, Perito ER, Mazariegos GV, Vanderwerken D, Segev DL, Gentry S. Liver Simulated Allocation Model Does Not Accurately Predict Organ Offer Decisions in Pediatric Liver Transplant Candidates [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-simulated-allocation-model-does-not-accurately-predict-organ-offer-decisions-in-pediatric-liver-transplant-candidates/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress