Prevalence of Diabetic Changes on Kidney Allograft Biopsies of Normoglycemic Simultaneous Pancreas-Kidney Transplant Recipients
Johns Hopkins University, Baltimore, MD
Meeting: 2021 American Transplant Congress
Abstract number: 410
Keywords: Biopsy, Hyperglycemia, Kidney/pancreas transplantation
Topic: Clinical Science » Pancreas » Pancreas and Islet: All Topics
Session Information
Session Time: 7:30pm-8:30pm
 Presentation Time: 7:50pm-8:00pm
Presentation Time: 7:50pm-8:00pm
Location: Virtual
*Purpose: Small studies suggest that achieving normoglycemia with simultaneous pancreas-kidney transplant (SPK) prevents the development of diabetic nephropathy (DN) among type 1 diabetics (T1DM). However, hemodynamic pathways, profibrotic cytokines, and genetic predisposition also contribute to the pathogenesis of DN and may not be reversed by an SPK. We sought to determine if diabetic changes (DC) occur in kidney graft biopsies of normoglycemic SPK recipients.
*Methods: We conducted a retrospective review of medical records of all SPK recipients at our center from 1996-2019. For our analysis, we included recipients with at least 1 kidney graft biopsy > 6 months after SPK and a functioning pancreas at the time of biopsy (defined as having a hemoglobin A1c < 6.5% without oral hypoglycemic agents or chronic insulin use). Our primary outcome was the prevalence of early structural DC namely glomerular basement membrane thickening and/or mesangial matrix expansion. Secondary outcomes included kidney graft outcomes. We expressed categorical data as absolute numbers (%) and continuous data as medians (interquartile range, IQR).
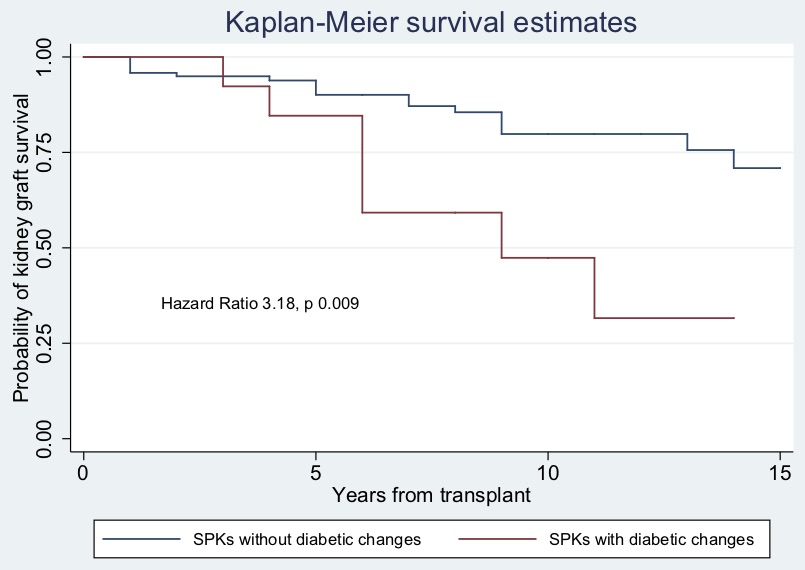
*Results: Of 150 T1DM SPK recipients, 43 had a kidney graft biopsy. 23 (53%) met inclusion criteria. Most of those excluded had pancreas failure. Baseline characteristics are shown in Table 1. 14/23 recipients (61%) had a biopsy showing early DC at a median of 34.5 months (18.7-101.7) after SPK. 5 (22%) had DN as part of the final pathologic diagnosis (median of 42 months after SPK, IQR 36-134). At the time of the first biopsy with DC, median serum creatinine was 1.7 mg/dl (1.35-2.24) and hemoglobin A1c was 5.4% (5.2-5.9). Median kidney graft follow-up was 102 months (60.5-159). During follow-up of the 14 recipients with DC, 8 (57%) had acute cellular rejection, 2 (14%) had antibody mediated rejection, and 8 (57%) progressed to kidney graft failure. Graph 1 shows the difference of kidney graft survival between recipients with DC versus those without.
*Conclusions: This is the first study that shows that DC (61%) and DN (22%) can recur after SPK despite good glucose control and is seen relatively early after transplant. This suggests that other mechanisms contribute to the development of DN after SPK.
| Age at transplant, (IQR) | 36 years (31.5-45) |
| Men (%) | 16 (70) |
| White (%) | 13 (56) |
| Body mass index at transplant (IQR) | 23.5 kg/m2 (22-24.8) |
| Deceased Donor (%) | 22 (96) |
| Thymoglobulin induction | 19 (82) |
| Maintenance immunosuppression: Prednisone + Tacrolimus |
23 (100) |
| Mycophenolate mofetil | 22 (96) |
To cite this abstract in AMA style:
Mejia C, Giannini G, Brennan DC, Rosenberg A, Alasfar S. Prevalence of Diabetic Changes on Kidney Allograft Biopsies of Normoglycemic Simultaneous Pancreas-Kidney Transplant Recipients [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/prevalence-of-diabetic-changes-on-kidney-allograft-biopsies-of-normoglycemic-simultaneous-pancreas-kidney-transplant-recipients/. Accessed February 18, 2026.« Back to 2021 American Transplant Congress