Identifying an Optimal Liver Frailty Index Cutoff to Predict Waitlist Mortality in Liver Transplant Candidates
1UCSF, SF, CA, 2Duke, Durham, NC, 3UPMC, Pittsburgh, PA, 4LLU, Loma Linda, CA, 5BSWH, Dallas, TX, 6Columbia, NY, NY, 7Northwestern, Chicago, IL, 8JHMI, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: A-167
Keywords: Liver transplantation, Mortality, Waiting lists
Session Information
Session Name: Poster Session A: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Frailty is associated with mortality in liver transplant (LT) waitlist candidates. We developed the Liver Frailty Index (LFI) to assess frailty in patients with cirrhosis that has been included in the American Society of Transplantation Frailty Toolkit for LT. To facilitate clinical decision-making using the LFI, we sought to identify an optimal LFI cutoff that predicts waitlist mortality.
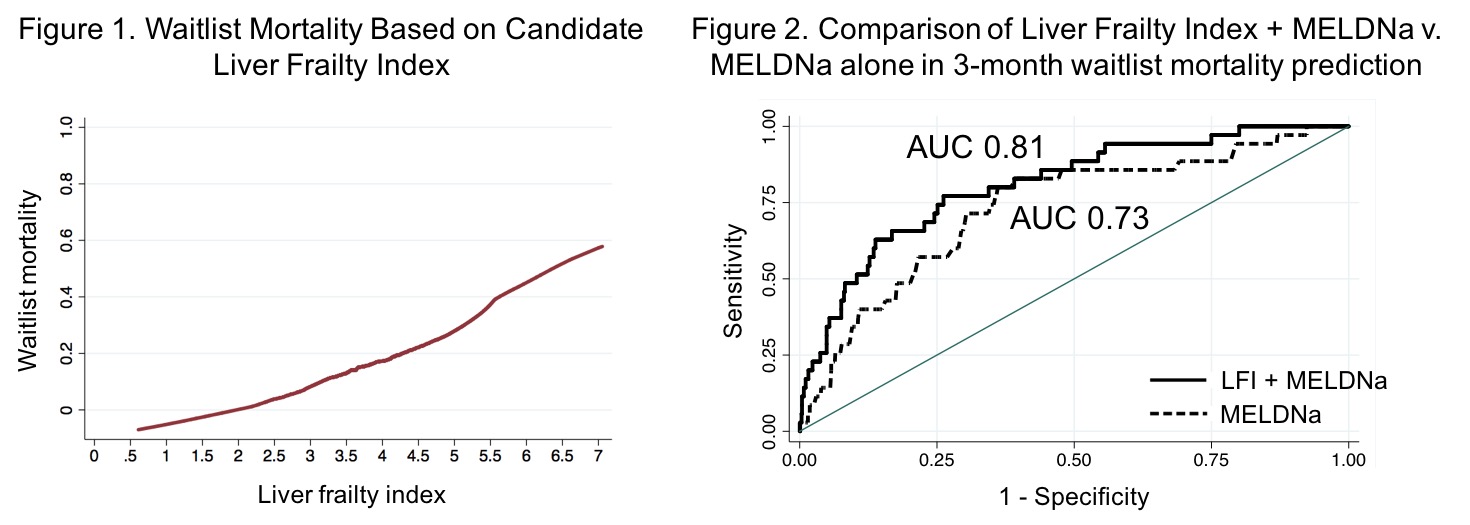
*Methods: Adults with cirrhosis awaiting LT without hepatocellular carcinoma at 8 U.S. LT centers with LFI assessments were included. Multivariable competing risk analysis and restricted cubic splines assessed the relationship between LFI and waitlist mortality (=death/delisting for sickness). We identified a single LFI cutoff by 2 approaches. We evaluated the fit of the competing risk models, searching for the LFI cutoff that gave the best model fit (as judged by the pseudo-log-likelihood). We then used the area under the ROC curve (AUC) in an analysis of waitlist mortality by 3, 6, and 12 months to find the optimal cutoff (Liu method). We used the AUC to compare the discriminative ability of LFI+MELDNa versus MELDNa alone in waitlist mortality prediction at 3 months.
*Results: Of 1,238 patients, 35 (3%), 77 (6%), and 127 (10%) experienced waitlist mortality at 3, 6, and 12 mo. LFI was predictive of waitlist mortality across a broad LFI range from 3.7 to 5.2; in other words, along this range, those with higher values experienced higher waitlist mortality. We observed a monotonic association between LFI and waitlist mortality (Fig 1). We identified an optimal LFI cutoff of 4.4 (95% CI: 3.9-4.8) for 3 mo, 4.2 (95% CI: 4.1-4.4) for 6 mo, and 4.2 (95% CI: 4.0-4.4) for 12 mo mortality. The AUC for prediction of 3 mo mortality for MELDNa was 0.73; the addition of LFI to MELDNa improved the AUC to 0.81 (Fig 2).
*Conclusions: LFI is predictive of waitlist mortality across a wide spectrum of LFI values. The optimal cutoff for LFI for waitlist mortality was 4.4 at 3 months and 4.2 at 6 and 12 months. The discriminative performance of LFI combined with MELDNa was substantially higher than MELDNa alone. Our data suggest that incorporating LFI with MELDNa can be used to more accurately represent waitlist mortality in cirrhosis patients to facilitate transplant decision-making and patient discussions.
To cite this abstract in AMA style:
Kardashian A, Ge J, McCulloch C, Kappus MR, Dunn MA, Duarte-Rojo A, Volk ML, Rahimi RS, Verna EC, Ganger DR, Ladner D, Dodge JL, Boyarsky B, McAdams-DeMarco M, Segev DL, Lai JC. Identifying an Optimal Liver Frailty Index Cutoff to Predict Waitlist Mortality in Liver Transplant Candidates [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/identifying-an-optimal-liver-frailty-index-cutoff-to-predict-waitlist-mortality-in-liver-transplant-candidates/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress