Efficacy of Single-Strength Trimethoprim-Sulfamethoxazole Thrice Weekly for Pneumocysitis Jirovecii Pneumonia Prophylaxis Post Liver Transplantation
A. Puing, A. Subramanian
Infectious Diseases and Geographic Medicine, Stanford University, Stanford, CA
Meeting: 2020 American Transplant Congress
Abstract number: D-151
Keywords: Infection, Liver, Prophylaxis
Session Information
Session Name: Poster Session D: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Current guidelines recommend Pneumocystis jirovecii pneumonia (PJP) prophylaxis for at least 6-12 months after liver transplant (LTx) with preferably Trimethoprim-sulfamethoxazole (TMP-SMX) at a daily dose of 80/400 mg (single-strength) or 160/800 mg (double-strength) three times weekly. Here we aimed to retrospectively examine our institutional experience using a lower dose, single-strength TMP-SMX thrice weekly for 12 months postLTx for PJP prophylaxis from 2012 to 2016.
*Methods: Retrospective cohort study of adult patients that underwent LTx at our institution from 01/2012-12/2016 and were discharged on PJP prophylaxis. Patients were followed for a year post-LTx. Baseline demographic, clinical, serological, and outcomes information were collected.
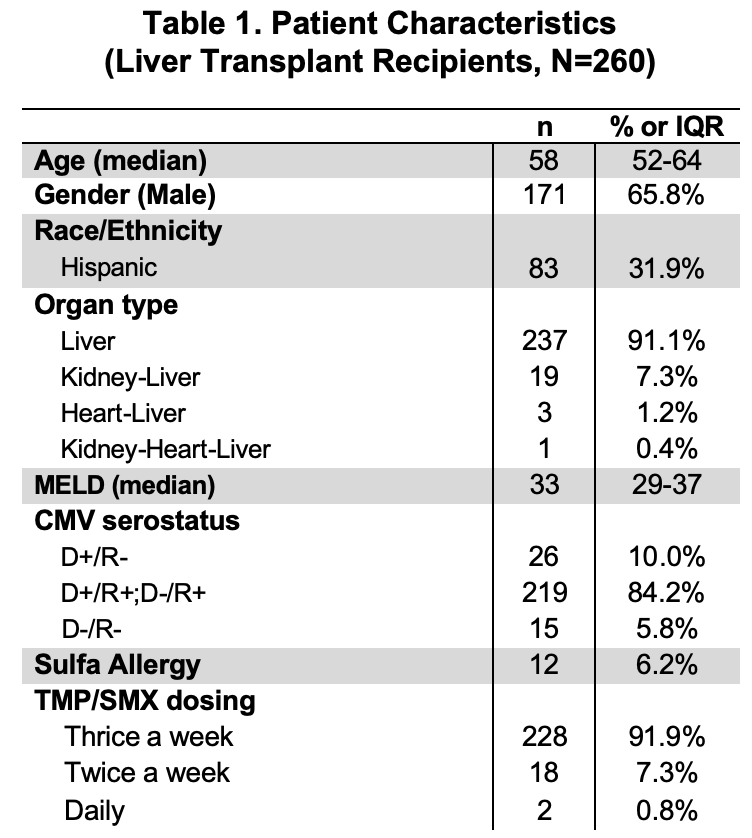
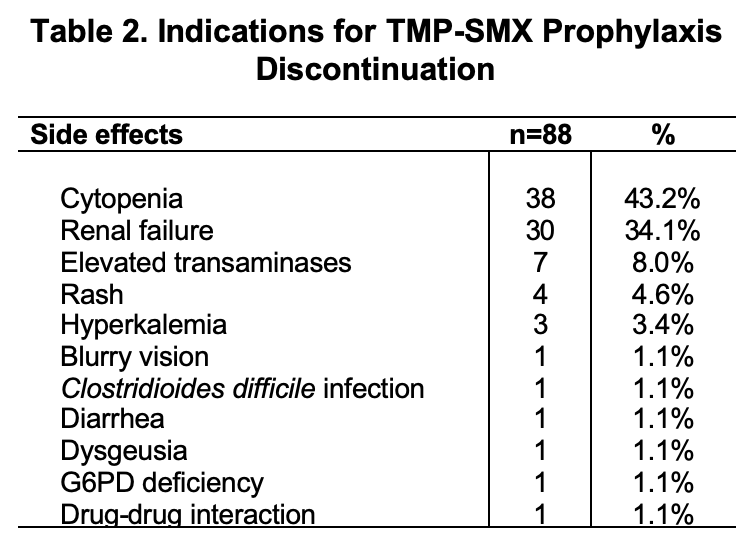
*Results: 260 LTx recipients met inclusion criteria. 248 (93.8%) of these patients were initially prescribed single-strength TMP-SMX for prophylaxis. 12 (6.2%) were prescribed alternative prophylaxis because of sulfa allergy. Of those receiving single-strength TMP-SMX, 228 (91.9%) took it thrice a week, 18 (7.3%) twice a week, and 2 (0.8%) daily. Patient characteristics are shown in Table 1. 88 (35.5%) patients discontinued TMP-SMX because of adverse effects. The most common reasons for TMP-SMX discontinuation or avoidance was development of cytopenia in 38 (43.2%) and elevated creatinine in 30 (34.1%) (Table 2). Of the 260 adult liver transplant recipients transplanted at our institution over a 5-year period ending in 12/2016, only 1 opportunistic infection (OI) was documented in the 1st-year post-LTx, namely toxoplasmosis in a patient 4 months post-LTx for hepatocellular carcinoma.
*Conclusions: This study shows that low-dose TMP-SMX thrice a week is relatively effective in preventing OI in LTx recipients during the first-year post-transplant. Cytopenia and elevated creatinine are relatively common in the postoperative period and may be multifactorial; when cytopenia or renal insufficiency improve, patients should be rechallenged with TMP-SMX. Further research is needed to clarify the optimal dosing of TMP-SMX to prevent PJP and other OIs while avoiding adverse drug reactions.
To cite this abstract in AMA style:
Puing A, Subramanian A. Efficacy of Single-Strength Trimethoprim-Sulfamethoxazole Thrice Weekly for Pneumocysitis Jirovecii Pneumonia Prophylaxis Post Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/efficacy-of-single-strength-trimethoprim-sulfamethoxazole-thrice-weekly-for-pneumocysitis-jirovecii-pneumonia-prophylaxis-post-liver-transplantation/. Accessed March 2, 2026.« Back to 2020 American Transplant Congress