Incidence, Risk Factors, and Kidney Transplant Outcomes Associated with Post-Transplant Diabetes Mellitus
R. F. Malik1, Y. Jia1, S. G. Mansour2, I. E. Hall2, M. D. Doshi2, P. P. Reese2, P. Singh2, M. N. Harhay2, F. L. Weng2, H. Thiessen Philbrook1, B. Schröppel2, T. Muthukumar2, J. S. Bromberg2, E. Akalin2, S. Mohan2, C. R. Parikh1
1Johns Hopkins University, Baltimore, MD, 2DDS Consortium, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: D-032
Keywords: Graft failure, Kidney transplantation, Post-transplant diabetes
Session Information
Session Name: Poster Session D: Kidney: Cardiovascular and Metabolic Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Post-Transplant Diabetes Mellitus (PTDM) is a common complication after kidney transplant (KT). Most prior studies are single-center with short follow-up and inconsistent outcome ascertainment. In a multi-center cohort, we studied the incidence and risk factors for PTDM, the effect of post-KT body mass index (BMI) trajectory on PTDM, and associations between PTDM and graft failure.
*Methods: We ascertained up to 5 years of transplant outcome data through detailed chart review for 1137 adult recipients receiving deceased donor kidneys from 13 transplant centers in 2010-2013. 505 (44%) were excluded due to the presence of pre-transplant diabetes, resulting in an analytic cohort of 632 patients. We defined PTDM as chart-documented diagnosis according to treating physicians. We used descriptive statistics to assess modifiable and non-modifiable PTDM risk factors and the relationship between BMI trajectory and PTDM. We assessed associations between PTDM and graft outcomes via time-dependent covariate cox models.
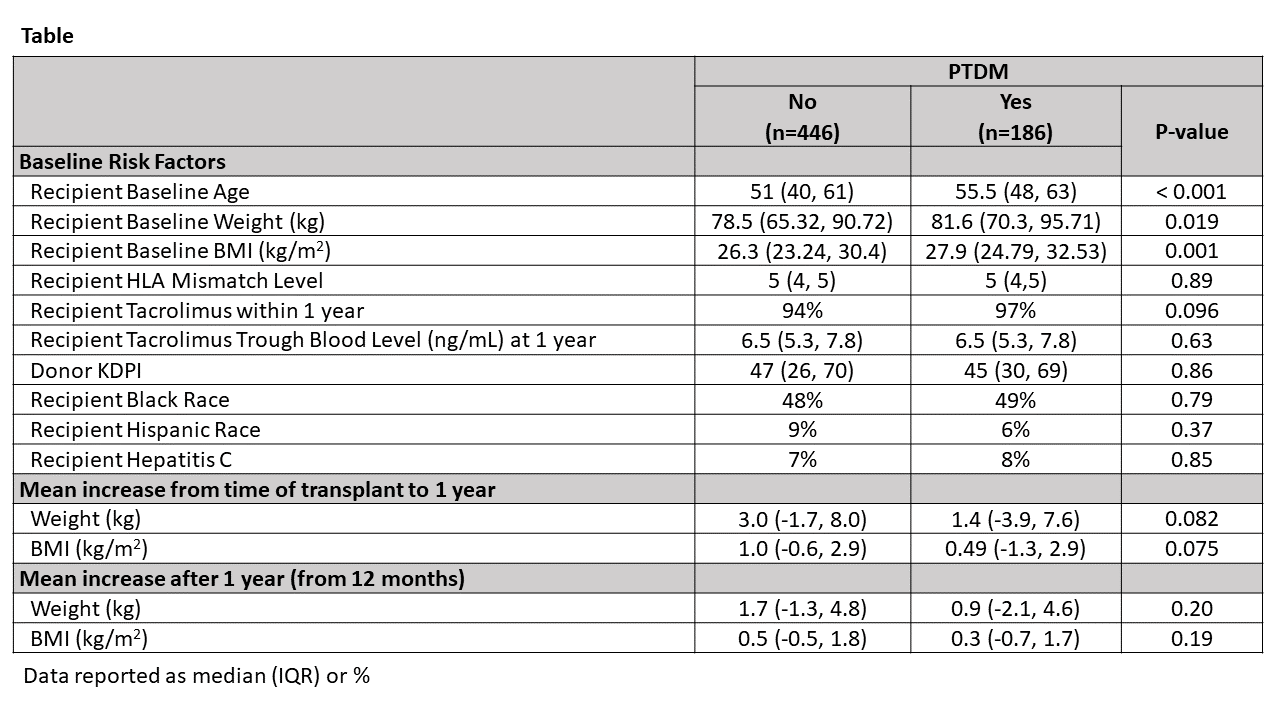
*Results: Mean recipient age was 52±14 years, 59% were male, and 49% were black. Median follow-up was 5 (IQR 3.8-5.0) years. 186 (29%) patients developed PTDM. About 50% of PTDM patients were diagnosed within the first 12 months of KT. 80 (43%) of recipients with PTDM were treated with insulin, 71 (38%) with pills only, and 35 (19%) had no documented diabetes medications. Independent baseline risk factors for PTDM included older recipient age (p<0.001) and higher BMI (p=0.001). Within the first year, overall median BMI rise was 1.2 kg/m2 (IQR 0, 2.5) and was similar in both PTDM and non-PTDM groups. Beyond 12 months post-KT, BMI rise slowed for both groups (Table). PTDM was not associated with all-cause graft failure [adjusted Hazard Ratio (aHR) 1.10 (95% CI: 0.78-1.55)], death-censored graft failure [aHR 0.85 (0.53-1.37)], or death [aHR 1.31 (0.84-2.05)].
*Conclusions: PTDM occurred commonly after KT. Higher baseline BMI was associated with PTDM, but not increasing BMI post-KT. Furthermore, our data do not demonstrate significant associations between PTDM and post-transplant graft failure outcomes.
To cite this abstract in AMA style:
Malik RF, Jia Y, Mansour SG, Hall IE, Doshi MD, Reese PP, Singh P, Harhay MN, Weng FL, Philbrook HThiessen, Schröppel B, Muthukumar T, Bromberg JS, Akalin E, Mohan S, Parikh CR. Incidence, Risk Factors, and Kidney Transplant Outcomes Associated with Post-Transplant Diabetes Mellitus [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/incidence-risk-factors-and-kidney-transplant-outcomes-associated-with-post-transplant-diabetes-mellitus/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress