Adult Liver Transplant Recipients Show Increased Fibrinolysis Resistance Compared with Pediatric Recipients: The Potential Impact of Anticoagulation between the Two Populations
University of Colorado, Aurora, CO
Meeting: 2020 American Transplant Congress
Abstract number: C-174
Keywords: Anticoagulation, Liver transplantation, Pediatric
Session Information
Session Name: Poster Session C: Liver: Pediatrics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Fibrinolytic changes in adult liver transplant patients have previously been demonstrated large transitions from excessive fibrinolysis (hyperfibrinolysis) to fibrinolysis resistance (shutdown) within 2 hours of graft reperfusion. These shifts in fibrinolysis remains unclear in pediatric transplant surgery. We hypothesize that pediatric liver transplant patients will transition to fibrinolysis resistance following graft reperfusion, similar to adults.
*Methods: Serial blood samples were obtained pre-operatively through post-operative (POD) day 5 in adult and pediatric liver transplant patients. Blood was assayed with thrombelastography to quantify fibrinolysis sensitivity and resistance to tPA mediated fibrinolysis by measuring the percent of clot degraded 30 minutes after maximum clot strength with the addition of tissue plasminogen activator (tPA) to the TEG cup. Pediatric patients (age less than 15) were contrasted to adult versus pediatric with Mann Whitney U test. A final analysis also included assessing patients that were treated with aspirin or heparin post operatively to assess if this intervention had an associated change in fibrinolysis post-op.
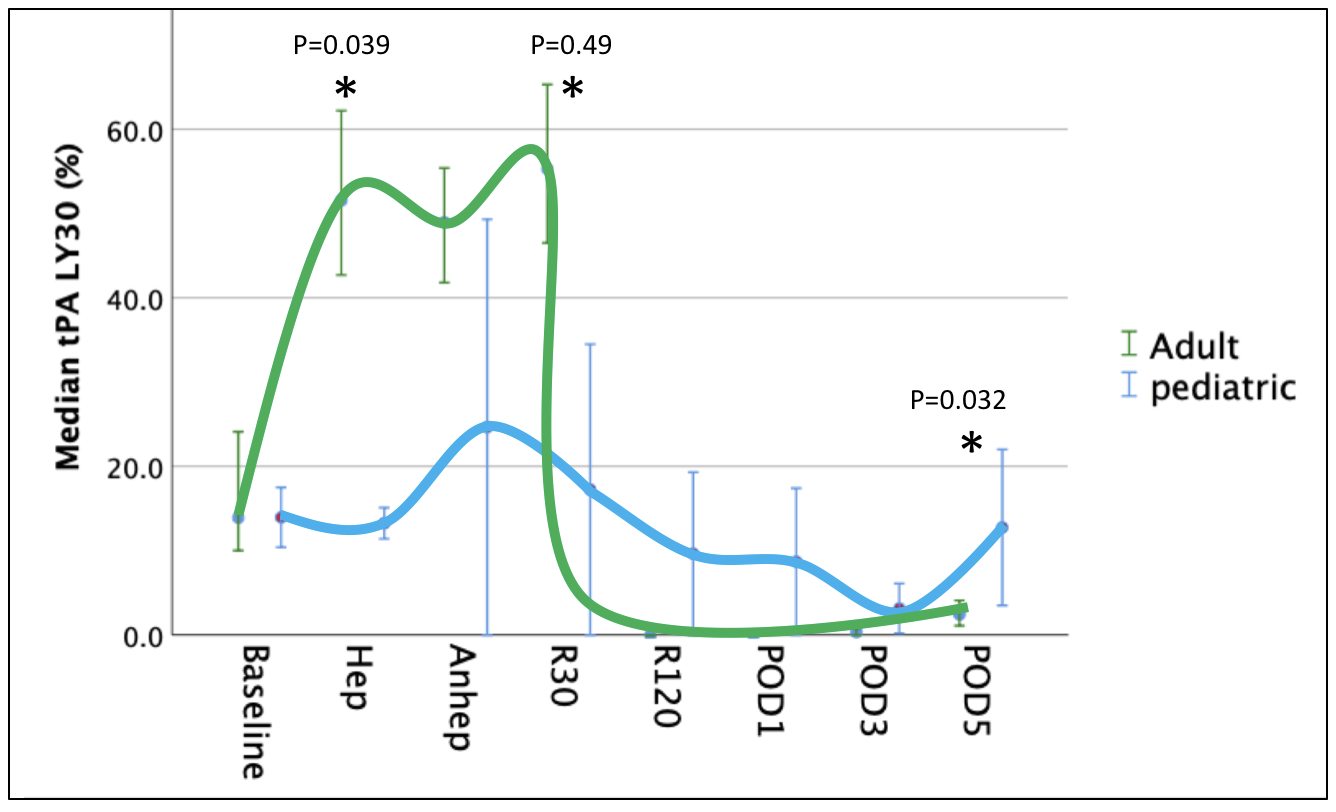
*Results: 59 patients included in the analysis. Of this cohort 9 were pediatric. The median MELD was 20. Fibrinolytic changes contrasted between adult and pediatric patients are depicted in the figure, which demonstrated that pediatric patients had less tPA sensitivity than adults during the recipient hepatectomy (p=0.041) and 30 minutes following reperfusion (p=0.049), but regained a higher sensitivity to fibrinolysis on POD 5 (p=0.032). Within the pediatric cohort 40% of patients were on post-op heparin or aspirin, while only 4% were on one of these medications in the adult population. When using a combination of adult and pediatric patients contrasting the use of post-op anticoagulants fibrinolysis was significantly increased in patients on these medications on POD 3 (4.2% vs 0.2% p=0.041) and POD 5 (8.5% vs 2.3% p=0.031) and closer to pre-operative levels.
*Conclusions: This preliminary analysis of pediatric liver transplant recpients supports that these patients have less extreme swings in fibrinolytic activity compared with adults and appear to recover from fibrinolysis resistance earlier than adults. This same association was found in liver transplant patients that were treated with aspirin or heparin post operatively. Ongoing investigation is warranted while controlling for post-operative anticoagulant medications.
To cite this abstract in AMA style:
Moore HB, Nydam T, Choudhury R, Schulick A, Walker C, Wachs M, Adams MA. Adult Liver Transplant Recipients Show Increased Fibrinolysis Resistance Compared with Pediatric Recipients: The Potential Impact of Anticoagulation between the Two Populations [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/adult-liver-transplant-recipients-show-increased-fibrinolysis-resistance-compared-with-pediatric-recipients-the-potential-impact-of-anticoagulation-between-the-two-populations/. Accessed January 29, 2026.« Back to 2020 American Transplant Congress