Delayed Introduction of Mammalian Inhibitors of Rapamycin (mTOR) Post Kidney Transplantation Might Avoid the Chronic Nephrotoxicity of Calcineurin Inhibitors. Herein We Are Reporting an Eight-Years Single Center Experience of mTOR-Based Immunosuppression Regimen in Comparison with Cyclosporin-Based Regimen
1Medicine-Nephrology, University of Tennessee Health Science Center, Memphis, TN, 2Medicine-Nephrology, Minia Nephrology Hospital, Minia University, Minia, Egypt
Meeting: 2020 American Transplant Congress
Abstract number: C-118
Keywords: Calcineurin, Donation, Immunosuppression, Kidney transplantation
Session Information
Session Name: Poster Session C: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Delayed introduction of mTOR inhibitors post kidney transplantation might avoid the chronic nephrotoxicity of CNI: eight-years single center experience.
*Methods: This is a retrospective analysis of all patients who received a kidney transplant at Nasr city Insurance and Nile Badrawy Hospitals from 2011 to 2018. All transplant recipients received a graft from Living unrelated donor, panel reactive antibody zero and no donor specific antibody. Uni- and multi-variate analysis were done to compare between mammalian target of rapamycin inhibitors (mTOR-I) based regimen and cyslosporin inhibitor (CNI)-based regimen.
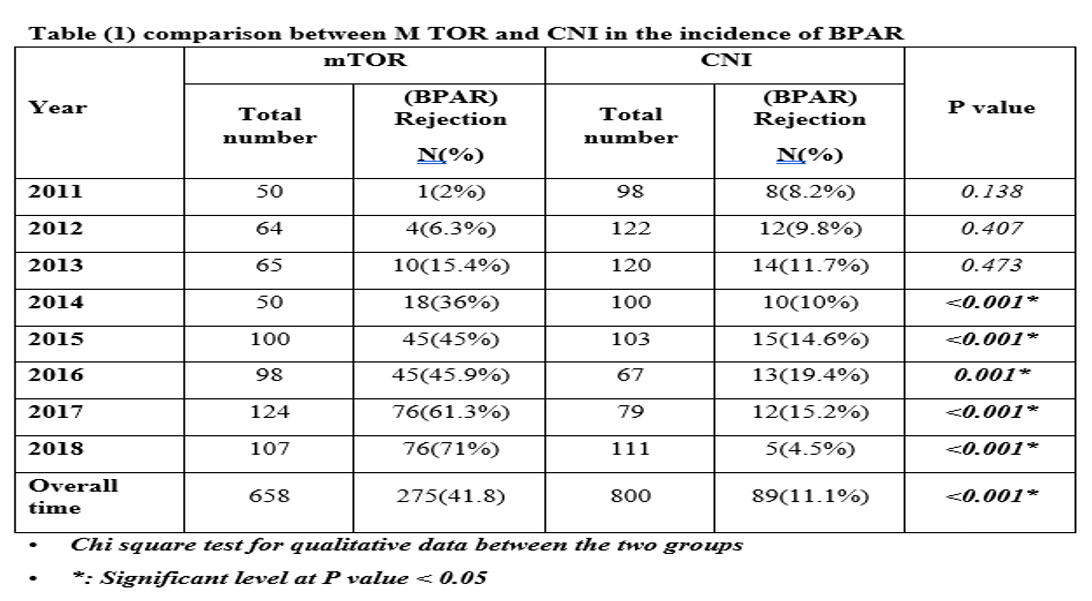
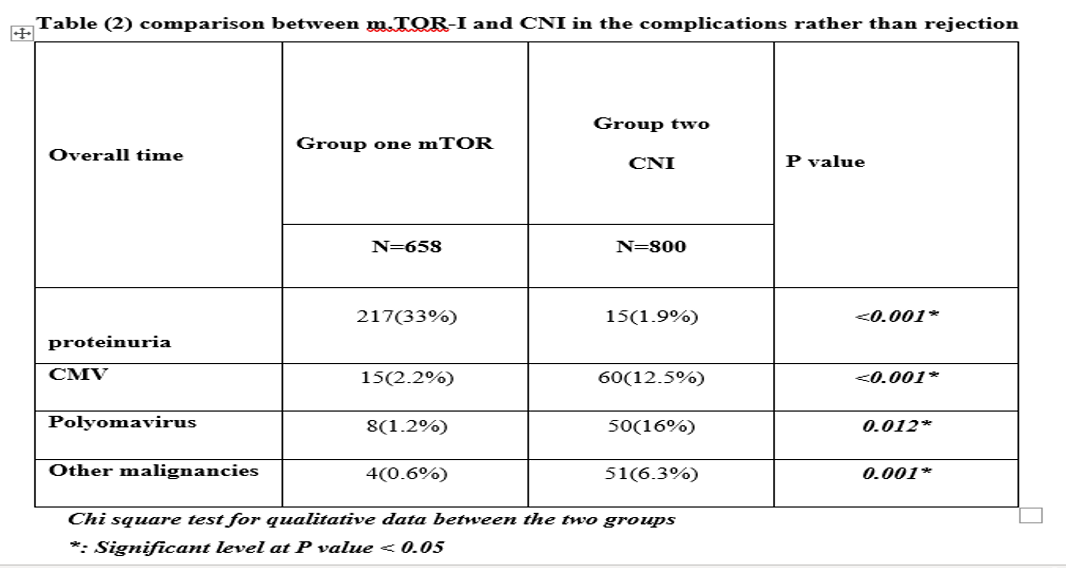
*Results: We identified 1458 renal transplant recipients who underwent living unrelated donor kidney transplant. All patient received Induction with anti-thymocyte globulin then were maintained on mycophenolate mofetil (MMF)-CNI-prednisone for at least 6 months. The patients were classified into two groups: *Group I: 658 patients on mTOR-I (sirolimus or everolimus), who were shifted from CNI to mTOR-I due to different causes. Group II: 800 patients on CNI (cyclosporin or tacrolimus). There were 237(36%) males and 421(64%) females in group I, 400 (50%) males and 400 (50%) females in group II. The mean age was 45.64 years for the group I, and 48.75 years for group II. There was significant statistical difference as regard biopsy proven acute rejection (BPAR) between group I (41.8%) and group II (11.1%0 (p<0.001). Also, there was significant difference between incidence of proteinuria (p<0.001); 33% in mTOR-I, and 1.9% with CNI (table 2). On the other hand, mTOR-I group had low incidence of BK and CMV infection (Table 2)
*Conclusions: mTOR-I based Immunosuppression regimen had higher risk of BPAR and statistically significant higher incidence of proteinuria in renal transplant recipients who were shifted from CNI to mTOR-I after 6 months post-transplantation, but low risk for BK and CMV infection.
To cite this abstract in AMA style:
Hassan WA, Tawfik HM. Delayed Introduction of Mammalian Inhibitors of Rapamycin (mTOR) Post Kidney Transplantation Might Avoid the Chronic Nephrotoxicity of Calcineurin Inhibitors. Herein We Are Reporting an Eight-Years Single Center Experience of mTOR-Based Immunosuppression Regimen in Comparison with Cyclosporin-Based Regimen [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/delayed-introduction-of-mammalian-inhibitors-of-rapamycin-mtor-post-kidney-transplantation-might-avoid-the-chronic-nephrotoxicity-of-calcineurin-inhibitors-herein-we-are-reporting-an-eight-years-si/. Accessed January 21, 2026.« Back to 2020 American Transplant Congress