Safely Increasing the Number of Renal Transplants Performed in a Small Center Through the Use of Acute Kidney Injury Donors
1Presbyterian Healthcare Services, University of New Mexico Health Sciences Center, Albuquerque, NM, 2Presbyterian Healthcare Services, Albuquerque, NM, 3Renal Medicine Associates, Presbyterian Healthcare Services, Albuquerque, NM
Meeting: 2020 American Transplant Congress
Abstract number: C-030
Keywords: Donors, marginal, Graft function, Kidney transplantation, Resource utilization
Session Information
Session Name: Poster Session C: Kidney Deceased Donor Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: New Mexico is medically underserved state with a significant end-stage renal disease population. This study aims to further demonstrate the safety of utilizing AKI donors to increase the number of allografts available for renal transplantation in a small transplant center.
*Methods: We retrospectively reviewed all renal transplants performed at the Presbyterian Healthcare Services Transplant Center from 2016 to 2019. Delayed graft function (DGF) was defined as the need for dialysis within 1 week post-transplant. Donor AKI was defined using the Acute Kidney Injury Network (AKIN) definition. Recipient serum creatinine (SCr) values were obtained from the time of last follow-up at the transplant center.
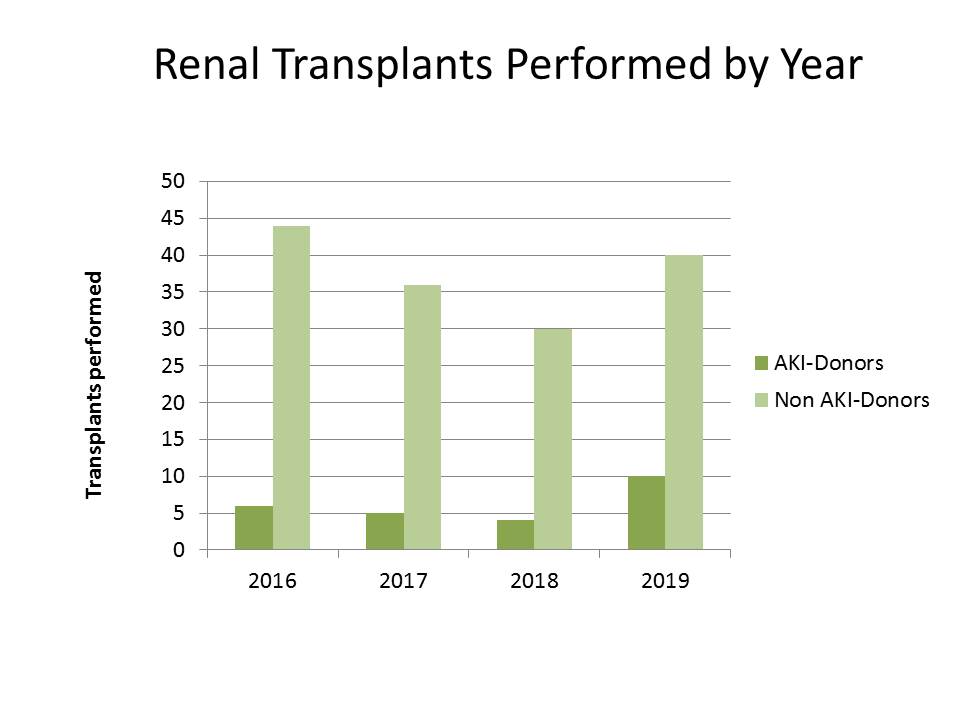
*Results: A total of 175 renal transplants were performed. 25 renal transplants were performed utilizing donor AKI kidneys and 150 renal transplants were performed utilizing non-AKI donor kidneys. Simultaneous kidney and pancreas transplants were not included in the study. 23 of the 25 (92%) AKI donor kidneys were classified as stage 3 AKI per AKIN definition. 2/25 AKI donor kidneys were classified as stage 2 AKI. Mean peak SCr in the donor AKI kidneys was 5.29 mg/dL (3.5-10.1mg/dL). Mean terminal SCr in the donor AKI kidneys was 5.03 mg/dL (2.19-10.1mg/dL). 6/25 (24%) of the AKI donor kidneys received hemodialysis prior to organ recovery. Mean AKI donor age was 29.4 years (15-41 years). Mean AKI donor kidney cold time was 21 hours 12 min (6 hours 38 min-33 hours 21 min). Mean AKI donor kidney warm time was 29.4 min (21-41min). 24/25 AKI donor kidneys were pumped. 15/25 (60%) of the AKI donor kidney recipients had DGF, in comparison to 21/150 (14%) of the non-AKI donor kidney recipients. At last follow up, the mean SCr for donor AKI kidney recipients was 1.19mg/dL (0.89-1.57mg/dL). There were no primary non-functions. One patient death with a functioning graft in the AKI donor kidney group occurred at 3 ½ years post-transplant, unrelated to transplant.
*Conclusions: AKI donors remain an underutilized method to reduce organ discard. Utilization of these kidneys is safe, and an effective way to increase access to transplantation and enhance program growth
To cite this abstract in AMA style:
Batie S, Eid K, Gabrys K, Barrantes F, Trujillo B, Kerr H. Safely Increasing the Number of Renal Transplants Performed in a Small Center Through the Use of Acute Kidney Injury Donors [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/safely-increasing-the-number-of-renal-transplants-performed-in-a-small-center-through-the-use-of-acute-kidney-injury-donors/. Accessed February 1, 2026.« Back to 2020 American Transplant Congress