Transpulmonary Gradient as a Predictor for Outcomes after Single Lung Transplantation in Patients with Pulmonary Hypertension
1University of Pittsburgh School of Medicine, Pittsburgh, PA, 2UPMC Department of Cardiothoracic Surgery, Pittsburgh, PA, 3UPMC Division of Pulmonary Medicine, Pittsburgh, PA
Meeting: 2020 American Transplant Congress
Abstract number: B-276
Keywords: Lung transplantation
Session Information
Session Name: Poster Session B: Lung: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: End stage lung disease is commonly associated with pulmonary artery hypertension (PAH). In a donor restrictive environment, offering patients single over double lung transplants can maximize organ utilization, reduce waiting list time and mortality. However, there remains to be a clinical consensus on how severe PAH must be to preclude single lung transplant (SLT) due to poor outcomes. We sought to investigate the predictive value of the transpulmonary gradient (TPG) in SLT in patients with end stage lung disease and pulmonary hypertension.
*Methods: We performed a retrospective cohort study utilizing the United Network for Organ Sharing (UNOS) database identifying all patients undergoing SLT from January 2005 to December 2017. TPG was calculated by subtracting mean capillary wedge pressure from mean pulmonary artery pressure, and patients were stratified based on their TPG score. Primary outcomes include 1-year survival assessed by a generalized linear mixed model (GLMM) where TPG value and transplant type were fixed effects, and transplant center was a random effect.
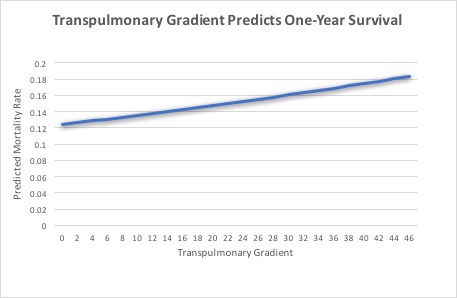
*Results: 6,926 SLT recipients were included in the analysis. Mean lung allocation score (LAS) for the cohort was 43.9. Mean length of stay for the entire cohort was 20.8 days. The GLMM showed TPG was predictive of 1-year survival (b = 0.011, t = 2.78, p < 0.001). When covarying for LAS and total bilirubin, a TPG >= 25 was associated with increased 1-year mortality risk for SLT (Exp(B) = 1.29, C.I. 1.01 – 1.64, t = 2.07, p = 0.039). The TPG >= 25 group had a trend towards longer length of stay compared to TPG < 25 (22.9 days vs. 21.0 days, p = 0.06). There was an increased 90-day mortality associated with patients with TPG >= 25 when compared to those with a TPG < 25 (Exp(B) = 1.42, C.I. 1.04-1.93, t = 2.23, p = 0.026). Once 90-day survival was reached, survival between the two groups was similar at 1 year (Exp(B) = 1.20, C.I. 0.93-1.55, t = 1.42, p = 0.16). Overall, the effect of TPG predicting mortality was found to have a 0.6% increase in mortality risk per 5 point TPG increase.
*Conclusions: An elevated preoperative TPG > 25 was associated with a decrease in 1-year survival in patients undergoing SLT. The use of preoperative TPG along with other marks of clinical status may help transplant centers in their decision of offering single vs double lung transplant in patients with pulmonary hypertension and end stage lung disease.
Figure 1.
To cite this abstract in AMA style:
Madde A, Chan E, Ryan J, Santos PReckDos, Morrell M, Luketich J, Sanchez P. Transpulmonary Gradient as a Predictor for Outcomes after Single Lung Transplantation in Patients with Pulmonary Hypertension [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/transpulmonary-gradient-as-a-predictor-for-outcomes-after-single-lung-transplantation-in-patients-with-pulmonary-hypertension/. Accessed February 4, 2026.« Back to 2020 American Transplant Congress