A Quality Improvement Project to Reduce the Risk of Alcohol Relapse after Liver Transplantation by Implementing a High-Risk Alcoholism Relapse Scale
R. V. Tholen1, E. Bundy2
1Transplant Nephrology, University of Maryland Medical Center, Baltimore, MD, 2School of Nursing, University of Maryland, Baltimore, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: B-246
Keywords: Alcohol, Liver failure, Liver transplantation, Psychosocial
Session Information
Session Name: Poster Session B: Psychosocial and Treatment Adherence
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Alcoholism is the leading cause of liver-related mortality worldwide. Liver transplantation is considered the only curative treatment for end-stage liver disease. Transplantation will reverse the complications of liver disease, but it does not treat underlying alcoholism or reduce the risk of relapse after transplant. In the United States, relapse rates are 20-50% among liver transplant recipients. Alcohol relapse after transplant has been identified as a problem among liver transplant recipients at a large urban academic transplant center in the United States. The purpose of this quality improvement project is to implement and evaluate the effectiveness of a High-Risk Alcoholism Relapse (HRAR) Scale to screen and identify patients at high-risk for relapsing after transplantation.
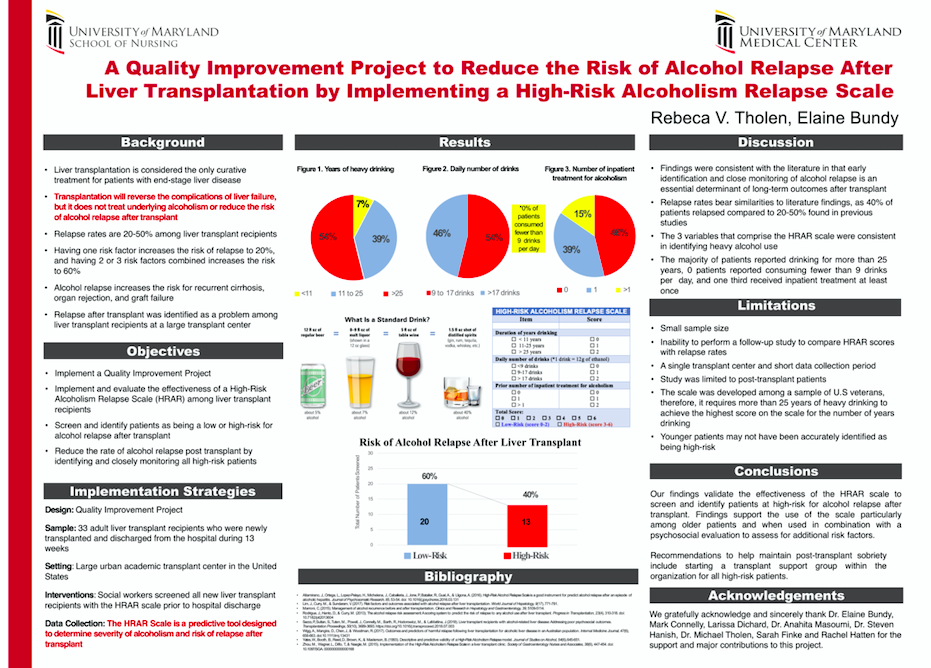
*Methods: The HRAR Scale is a predictive tool designed to determine severity of alcoholism and risk of relapse after transplant. It consists of three variables identified as having the highest predictive power for early relapse including, daily number of drinks, history of previous inpatient treatment for alcoholism, and number of years of heavy drinking. The scale was used to screen new adult liver transplant recipients prior to hospital discharge.
*Results: Descriptive statistics revealed 33 patients were newly transplanted and screened with the scale prior to hospital discharge. Forty percent of patients (n=13) were identified as being a high-risk for relapse and 60% low-risk (n=20). Fifty-four percent reported drinking nine to 17 drinks per day, and zero patients consumed fewer than nine drinks per day. Fifty-four percent reported drinking more than 25 years. One third of high-risk patients received inpatient treatment for alcoholism at least once.
*Conclusions: Early identification and close monitoring of alcohol relapse is an essential determinant of long-term outcomes after transplantation. Findings validate the effectiveness of the scale to screen and identify patients at high-risk for post-transplant relapse. Results support the scale as a more efficient method to identify heavy alcohol use than other screening methods. Recommendations for future studies include performing a follow-up study to compare HRAR results with relapse rates. Recommendations to help maintain post-transplant sobriety include starting a transplant support group within the organization for all high-risk patients.
To cite this abstract in AMA style:
Tholen RV, Bundy E. A Quality Improvement Project to Reduce the Risk of Alcohol Relapse after Liver Transplantation by Implementing a High-Risk Alcoholism Relapse Scale [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/a-quality-improvement-project-to-reduce-the-risk-of-alcohol-relapse-after-liver-transplantation-by-implementing-a-high-risk-alcoholism-relapse-scale/. Accessed January 9, 2026.« Back to 2020 American Transplant Congress