Opioid Prescription Pattern and Risk Factors Associated with Opioid Use after Living Donor Hepatectomy in the US
M. Nguyen1, L. Vest2, Z. Zhang2, V. Whittaker3, M. Schnitzler1, D. Axelrod4, H. Randall1, C. Varma1, J. Snyder5, B. Kasiske5, D. Segev6, M. McAdams Demarco7, G. Hess8, K. Lentine2
1Department of Surgery, Saint Louis University, Saint Louis, MO, 2Department of Medicine, Saint Louis University, Saint Louis, MO, 3Department of Surgery, New York Medical College, New York, NY, 4Department of Surgery, University of Iowa, Iowa City, IA, 5SRTR, Minneapolis, MN, 6Department of Surgery, Johns Hopkins University, Baltimore, MD, 7Johns Hopkins University, Baltimore, MD, 8Drexel University, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: B-158
Keywords: Liver transplantation, Living donor, Living-related liver donors, Pain
Session Information
Session Name: Poster Session B: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Opioids are the cornerstone of acute pain management after living donor hepatectomy. Their misuse poses the danger of chronic abuse. How this affects living liver donors is unknown in the opioid epidemic era. We investigated opioid prescription patterns and risk factors associated with opioid use after living donor hepatectomy in the US
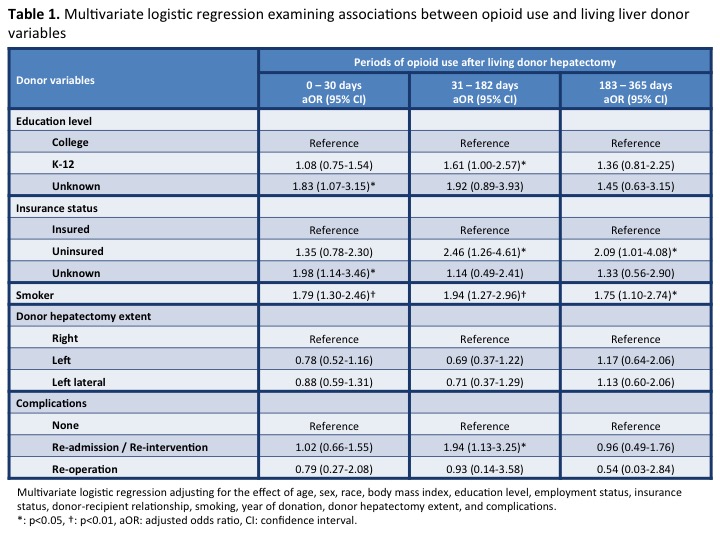
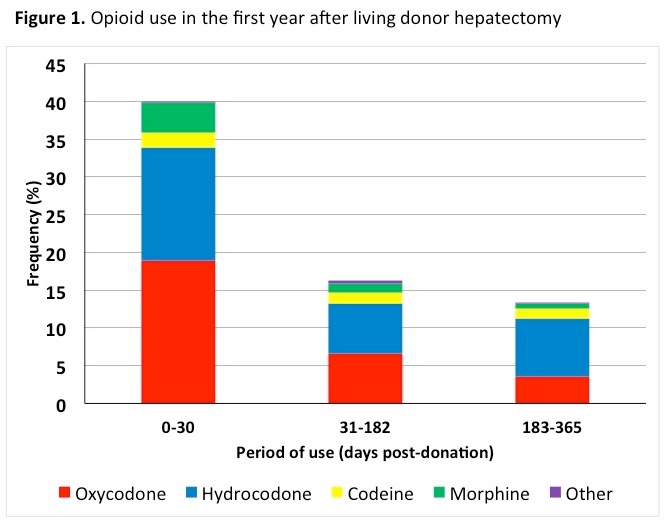
*Methods: Scientific Registry of Transplant Recipients data were combined with US pharmaceutical claims data (2007-2015) to determine opioid prescription patterns among 896 living liver donors at 0-30, 31-182, and 183-365 days post-donation. Associations between opioid use and donor variables were examined with multivariate logistic regression.
*Results: Opioid prescription filling among living liver donors was 40%, 16%, and 13% at 0-30, 31-182, and 183-365 days post-donation. The preferred opioid was oxycodone at 0-30 days, shifting to hydrocodone at 183-365 days (Figure 1). Right lobe, left lobe, or left lateral segment donation did not influence opioid use, nor did re-operation. Opioid use was increased at 31-182 days in donors who were re-admitted or underwent non-operative interventions. Demographic variables associated with increased opioid use beyond 0-30 days included white race, smoking, lower education level, and uninsured status (Table 1).
*Conclusions: We showed that 13%-16% of living liver donors required opioids beyond the acute pain phase post-hepatectomy with a preference shift from oxycodone to hydrocodone. Identified demographic and clinical risk factors could prove useful in developing targeted strategies to minimize opioid use in future living liver donors.
To cite this abstract in AMA style:
Nguyen M, Vest L, Zhang Z, Whittaker V, Schnitzler M, Axelrod D, Randall H, Varma C, Snyder J, Kasiske B, Segev D, Demarco MMcAdams, Hess G, Lentine K. Opioid Prescription Pattern and Risk Factors Associated with Opioid Use after Living Donor Hepatectomy in the US [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/opioid-prescription-pattern-and-risk-factors-associated-with-opioid-use-after-living-donor-hepatectomy-in-the-us/. Accessed February 24, 2026.« Back to 2020 American Transplant Congress