Shorter Waiting Time Was Associated with Higher Risk of Recurrence of Hepatocellular Carcinoma in Liver Transplantation
1Transplant and Hepatobiliary Surgery, Henry Ford Hospital, Detroit, MI, 2Gastroenterology and Hepatology, Henry Ford Hospital, Detroit, MI
Meeting: 2020 American Transplant Congress
Abstract number: B-140
Keywords: Hepatocellular carcinoma, Liver transplantation, Waiting lists
Session Information
Session Name: Poster Session B: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Liver transplantation (LT) is an established treatment option for hepatocellular carcinoma (HCC). After 6-month waiting rule was implemented, the impact of wait-listing (WL) time on recurrence of HCC has not been well investigated. The aim of study is to analyze the risk factors and evaluate the effect of WL time on recurrence of HCC.
*Methods: From 2013 to 2019, 173 HCC patients who underwent LT at Henry Ford Hospital were enrolled. Risk factors of post-transplant recurrence of HCC were analyzed. We specifically evaluated the impact of WL time on recurrence of HCC, therefore divided all patients into WL<120 days (Group 1, n=72) and WL≥120 days groups (Group 2, n=100) (no record in 1 patient), and compared patient, tumor demographics and cumulative incidence of HCC recurrence.
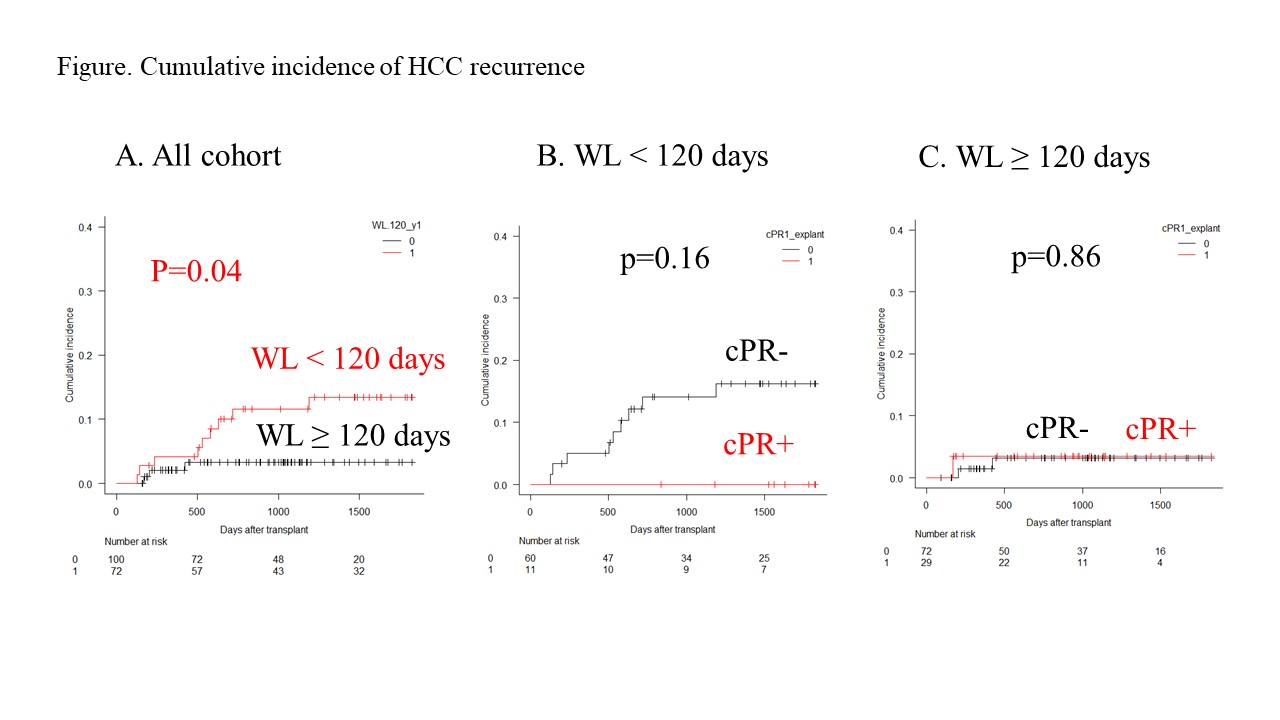
*Results: Post-transplant recurrence was found in 7.5% (13/173) with a median follow-up period of 35.2 months post-transplant. Univariate Cox regression analysis revealed that AFP at LT (hazard ratio [HR] 7.39, p=0.02), exceeding Milan criteria in explant pathology (HR 10.25, p=0.002), microvascular invasion (mVI) (HR 7.97, p<0.001), and WL<120 days (HR 3.66, p=0.049) were significant risk factors whereas age, gender, era of 6-month waiting rule, worst tumor differentiation, surgical parameters (duration of operation, ischemia time, amount of RBC) were not identified as risk factors. In Group 1, AFP at LT was relatively higher, the proportion of patients with complete pathological response (cPR) was significantly lower (15.5% vs 29.0%, p=0.04) compared to Group 2, whereas final MELD calculated score, number of locoregional therapies, the proportion of patients who exceeded Milan criteria both at LT and in explanted liver, those with mVI, and poor differentiated HCC were not different between 2 groups. Cumulative incidence of HCC recurrence was significantly higher in Group 1 (p=0.04, Figure A). In Group 1, cumulative incidence of HCC recurrence tended to be higher in patients without cPR than in those with cPR (p=0.16, Figure B) whereas, in Group 2, there was no difference between those with and without cPR (Figure C).
*Conclusions: Shorter waiting-time was associated with higher risk of post-transplant recurrence of HCC which could be attributable to incomplete bridging therapy. In the era of mandatory 6-month waiting rule, adequate pretransplant HCC treatments would decrease a risk of post-transplant HCC recurrence.
To cite this abstract in AMA style:
Kitajima T, Nagai S, Moonka D, Yeddula S, Rizzo O, Kavousi M, Salgia R, Rizzari M, Collins K, Yoshida A, Abouljoud MS. Shorter Waiting Time Was Associated with Higher Risk of Recurrence of Hepatocellular Carcinoma in Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/shorter-waiting-time-was-associated-with-higher-risk-of-recurrence-of-hepatocellular-carcinoma-in-liver-transplantation/. Accessed February 25, 2026.« Back to 2020 American Transplant Congress