Frailty Predicts Increased Length of Stay after Kidney Transplantation: An Implementation Study
J. Schaenman, B. Hale-Durbin, C. Lee, N. Ventigan, S. Jaladanki, L. Shih, B. Abdalla, R. Ahn, S. Chang, M. Dunbar-Forrest, H. A. Gritsch, G. Danovitch, D. Goldwater
David Geffen School of Medicine at UCLA, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: B-103
Keywords: Age factors, Elderly patients, Kidney transplantation, Screening
Session Information
Session Name: Poster Session B: Kidney Psychosocial
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Our objective was to implement a standardized an assessment of physical frailty and other aging-associated syndromes during routine evaluation of kidney transplant candidates over age 55, to provide additional information during candidacy evaluation for older patients at risk for post-transplant complications.
*Methods: We developed a tool that uses multiple standardized measures to assess geriatric syndromes, including: Fried Frailty Phenotype (FFP), the Short Physical Performance Battery (SPPB), Activities of Daily living (ADLs), cognitive function (mini-Cog), and fall-risk. To maximize time efficiency, the assessment is designed to be completed in two steps: 1) self-reported survey responses for patients to answer in the waiting room and 2) performance testing administered by a health- care professional.
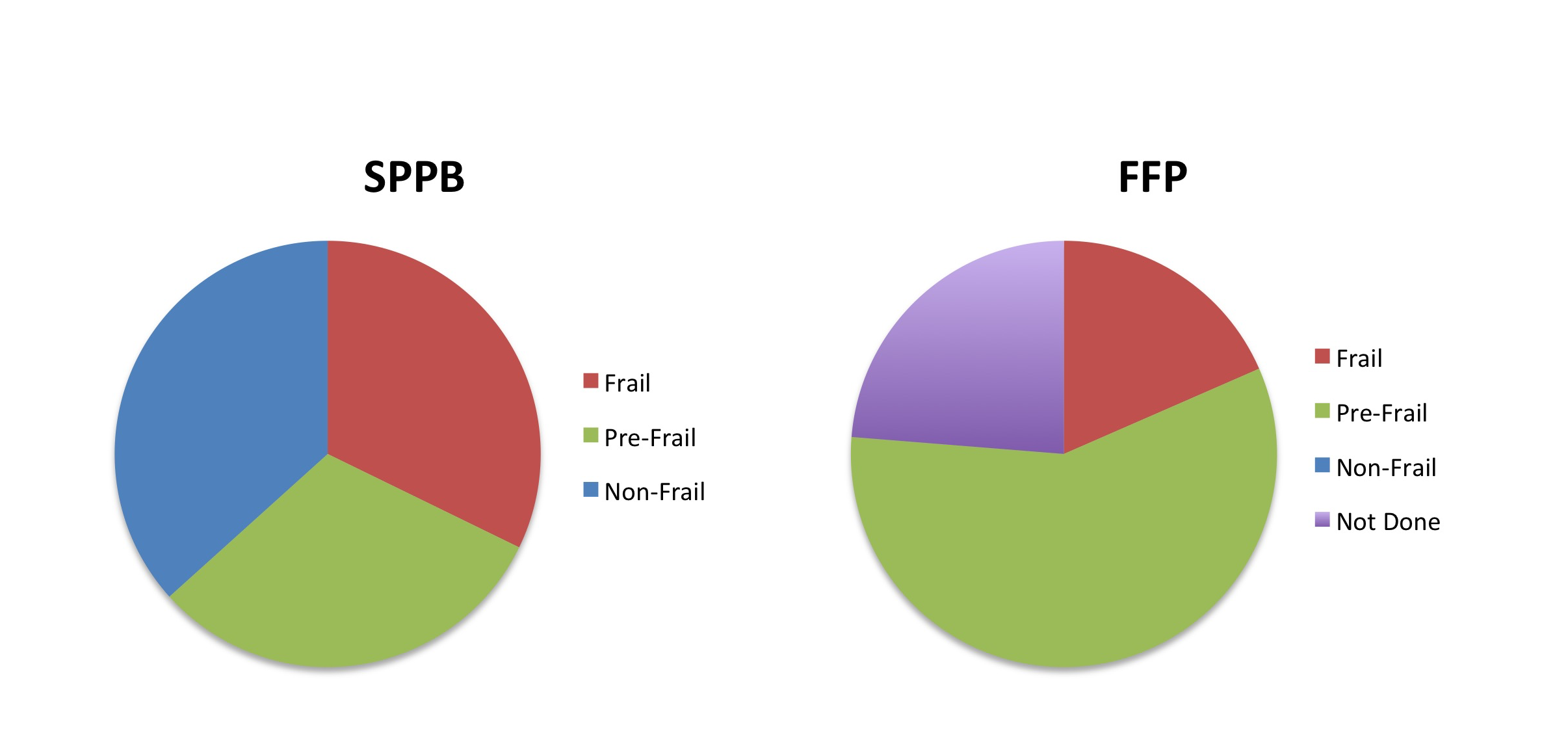
*Results: The assessment protocol became part of standard practice in April 2018. Total LVN plus physician time needed for administration is approximately 10 minutes per patient. We present the results of the assessment of the first 90 patients. Median patient age was 61 (range 55-79), and median BMI was 27 (range 18-40). The distribution of assessments by SBBP was 32% Frail, 31% Pre-Frail, and 37% Frail (Figure). For FFP assessment, 24% were frail and 76% Pre-Frail, while 31% did not undergo this assessment. 41 patients underwent transplantation, and 3 patients died. Median length of stay (LOS) after transplant was 5.5 (range 3-25). 33 patients were readmitted. SPPB was significantly associated with death (p=0.031). SPPB was also significantly associated with LOS (p=0.012). In contrast, frailty as assessed by FFP was not associated with death, although there was a trend towards association with increased LOS (p=0.088). A trend was observed towards characterization as Frail or Pre-Frail compared with Non-Frail by SPPB and hospital readmission in the first 3 months after transplantation (p=0.070).
*Conclusions: Through a streamlined, team-based effort, we were able successfully integrate evaluation of frailty and other aging-associated risk factors into patient assessment during outpatient clinic assessment. Future studies will evaluate the association between frailty and cognitive function, ADLs, and fall risk, and whether frailty evaluation by SPPB provides superior clinical prediction over FFP in this patient population.
To cite this abstract in AMA style:
Schaenman J, Hale-Durbin B, Lee C, Ventigan N, Jaladanki S, Shih L, Abdalla B, Ahn R, Chang S, Dunbar-Forrest M, Gritsch HA, Danovitch G, Goldwater D. Frailty Predicts Increased Length of Stay after Kidney Transplantation: An Implementation Study [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/frailty-predicts-increased-length-of-stay-after-kidney-transplantation-an-implementation-study/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress