Liver Transplant Waitlist Mortality is Not Associated with Urbanicity
1Surgery, Massachusetts General Hospital, Boston, MA, 2Surgery, Sinai Hospital of Baltimore, Baltimore, MA, 3Harvard School of Public Health, Boston, MA, 4Surgery, Brigham and Women's Hospital, Boston, MA
Meeting: 2020 American Transplant Congress
Abstract number: A-250
Keywords: Allocation, Liver transplantation, Outcome, Waiting lists
Session Information
Session Name: Poster Session A: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Because of geographic disparity in transplant rates and organ usage, distance-based liver distribution has been proposed to replace Donor Service Area based distribution. However, there is some concern that this policy will disadvantage rural populations when mixed with urban populations in a match run, because issues with access to care could place rural patients at higher risk of death, even at the same MELD score. We therefore aimed to investigate the impact of urbanicity on wait list mortality among liver transplant candidates with similar MELD scores.
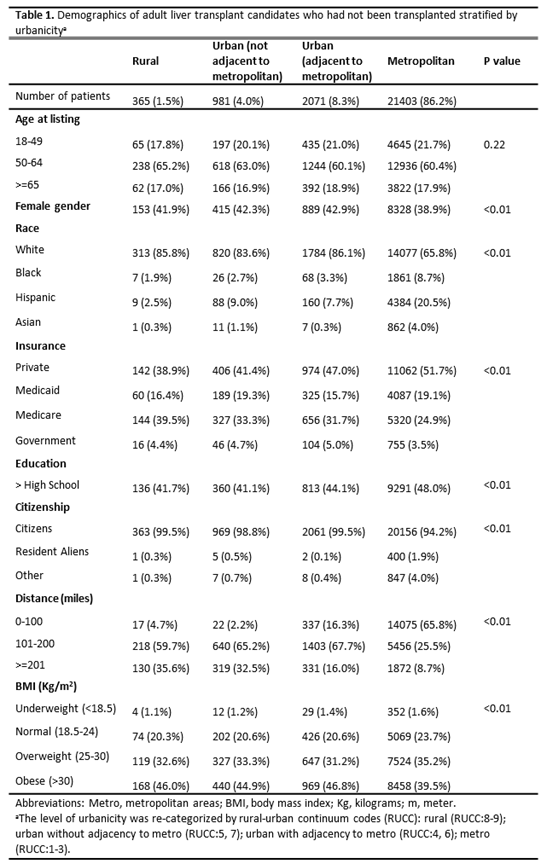
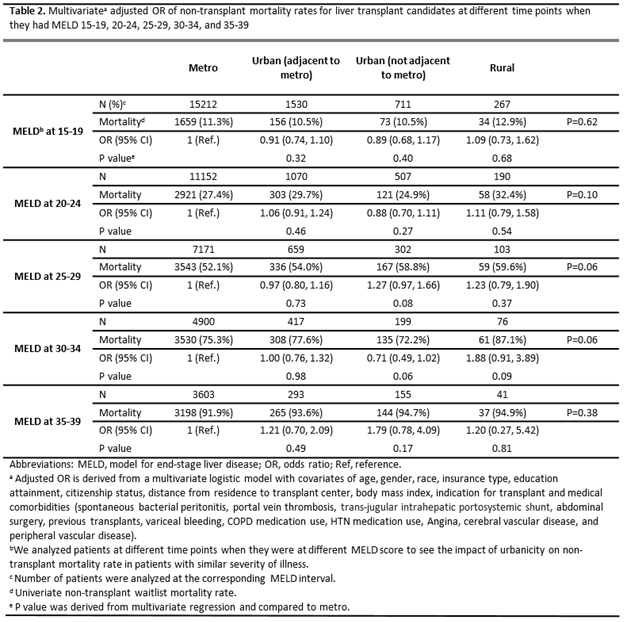
*Methods: We included adult transplant candidates who were on the waitlist 2010-2019, using the Scientific Registry of Transplant Recipients (SRTR). Our primary outcome was mortality rates within certain MELD score ranges among patients who did not receive a transplant, comparing urbanicity using zip code of residence, defined by rural-urban continuum codes (RUCC). Multivariate logistic regression was used to adjust for social and medical factors.
*Results: 24,820 patients, 365 (1.5%) living in rural areas, were analyzed (table 1). Compared to patients living in metropolitan areas, rural patients were more likely to be women (41.9% vs 38.9%), be white (85.8% vs 65.8%), US citizens (99.5% vs 94.2%), live >=200 miles away from the listed center (35.6% vs 8.7%), and less likely to be private insurance holders (38.9% vs 51.7%). After adjusting for demographic and medical factors, there were no significant differences in mortality between metro and rural patients with similar severity of illness (table 2).
*Conclusions: We found no difference in mortality rates of wait list candidates not receiving a transplant between rural and urban patients with similar severity of illness. Patients at higher risk due to poor access to care may not even be making it to the wait list. Improving access for rural patients and implementing distance-based liver allocation could have complementary roles in mitigating geographic disparity in access to liver transplantation.
To cite this abstract in AMA style:
Chen Y, Hung Y, Hsu Y, Crescenzo Cde, Rickert C, Adler J, Chang D, Yeh H. Liver Transplant Waitlist Mortality is Not Associated with Urbanicity [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-transplant-waitlist-mortality-is-not-associated-with-urbanicity/. Accessed January 20, 2026.« Back to 2020 American Transplant Congress