Epidemiology of Invasive Fungal Infections in Heart Transplant Recipients
A. Couture-Cossette1, A. Puing1, A. Multani2, O. Quintero1, A. K. Subramanian1, E. Henricksen3, R. Lee1, Y. Moayedi4, K. Khush5, J. J. Teuteberg5, D. Y. Ho1
1Department of Infectious Diseases and Geographic Medicine, Stanford University, Stanford, CA, 2Department of Infectious Diseases, UCLA, Stanford, CA, 3Pharmacy, Stanford Healthtcare, Stanford, CA, 4Department of Cardiology, UHN, Toronto, ON, Canada, 5Division of Cardiology, Department of Medicine, Stanford University, Stanford, CA
Meeting: 2020 American Transplant Congress
Abstract number: A-187
Keywords: Fungal infection, Heart, Infection, Prophylaxis
Session Information
Session Name: Poster Session A: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The incidence and epidemiology of invasive fungal infections (IFI) after heart transplantation (HTx) are influenced by changes in environmental exposures, immunosuppression, and prophylaxis practices. Despite this, antifungal prophylaxis is not uniform amongst HTx programs. The purpose of this study was to examine the incidence and nature of IFIs after HTx and assess the impact of prophylaxis on breakthrough IFIs.
*Methods: Retrospective analysis of 338 patients followed at an academic center after HTx (1/2008-12/2018). Universal itraconazole prophylaxis for 3 months was used if no contra-indications were present. Cases were identified and data was obtained from a comprehensive transplant patient database. IFIs were defined per EORTC/MSG consensus group criteria. Primary outcome was incidence of proven/probable IFI. Secondary outcomes were incidence of IFI while receiving antifungal prophylaxis (breakthrough) and outcome of IFI (resolution, death and IFI-related death).
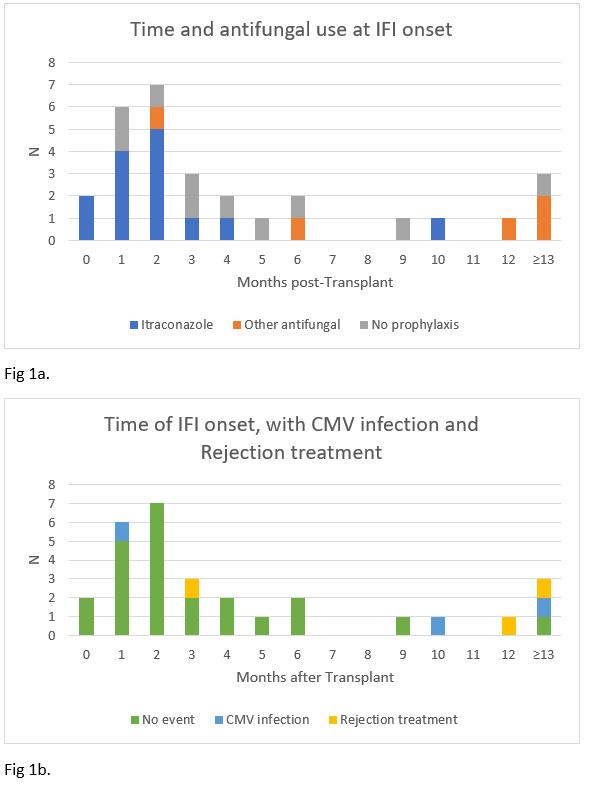
*Results: In 338 HTx patients, 29 episodes of IFI occurred in 25 patients (7.4%), of which 14 (48%) were breakthrough IFI in patients on itraconazole and 18 (62.1%) within 3 months of transplantation. Of 6 events occurring >6 months after transplantation, 4 (66%) followed rejection treatment and/or CMV infection. Excluding co-infection and relapse, fungal organisms were: 11 Aspergillus, 9 Candida, 3 Rhizopus, 2 Coccidoides, 1 Cryptococcus, 1 Paecilomyces and 1 Scedosporium. Patients with IFI frequently had diabetes (62.1%) or CKD (75.9%) and 44.8% of events occurred in patients on dialysis. One-year Mortality after IFI was 37.9%, with 27.6% IFI-related deaths.
*Conclusions: Despite use of prophylaxis, IFIs affect a small but significant proportion of HTx recipients. Almost half of cases were breakthrough IFIs. Most episodes were due to Aspergillus or Candida. The only endemic fungi were Coccidioides. While most episodes occur early after HTx, some occur later, often after immunocompromising events like CMV infection or treatment of rejection. There is a high prevalence of medical comorbidities or iatrogenic factors in patients with IFIs, which may have resulted in high mortality.
To cite this abstract in AMA style:
Couture-Cossette A, Puing A, Multani A, Quintero O, Subramanian AK, Henricksen E, Lee R, Moayedi Y, Khush K, Teuteberg JJ, Ho DY. Epidemiology of Invasive Fungal Infections in Heart Transplant Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/epidemiology-of-invasive-fungal-infections-in-heart-transplant-recipients/. Accessed February 13, 2026.« Back to 2020 American Transplant Congress