Different Prognostic Impact of Liver Transplantation According to Liver Disease Etiologies
Henry Ford Hospital, Detroit, MI
Meeting: 2020 American Transplant Congress
Abstract number: A-164
Keywords: Allocation, Liver transplantation, Mortality, Waiting lists
Session Information
Session Name: Poster Session A: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Disease specific background is not taken into consideration in the MELD-Na score based liver transplant (LT) allocation system. We hypothesized that optimal timing of LT might be different among liver disease etiologies. This study aims to evaluate possible discrepancy of prognostic impact of LT between major liver disease etiologies in the same MELD-Na score categories, including alcoholic-related liver disease (ALD); non-alcoholic steatohepatitis (NASH); hepatitis C virus cirrhosis (HCV) and Cholestatic Liver Diseases (CLD), limited to PBC and PSC.
*Methods: Data were obtained from the OPTN/UNOS registry. All adult patients with ALD, NASH, HCV or CLD registered for LT between Jan. 11, 2016 and Jun. 30, 2018 were selected. We excluded patients with overlapping etiologies, Status 1A, exception points, malignant liver tumors, re-transplantation and multivisceral transplant. Intention-to-treat survival (from registration through post-transplant) was evaluated in each disease group according to final MELD-Na score. Waitlist mortality and post-transplant mortality were set as endpoints. Cox regression analysis that modeled LT as a time dependent covariate was created to estimate prognostic impact of LT, which is considered treatment effects of LT. Risks were adjusted for patient characteristics, including age, gender, encephalopathy, ascites, and diabetes.
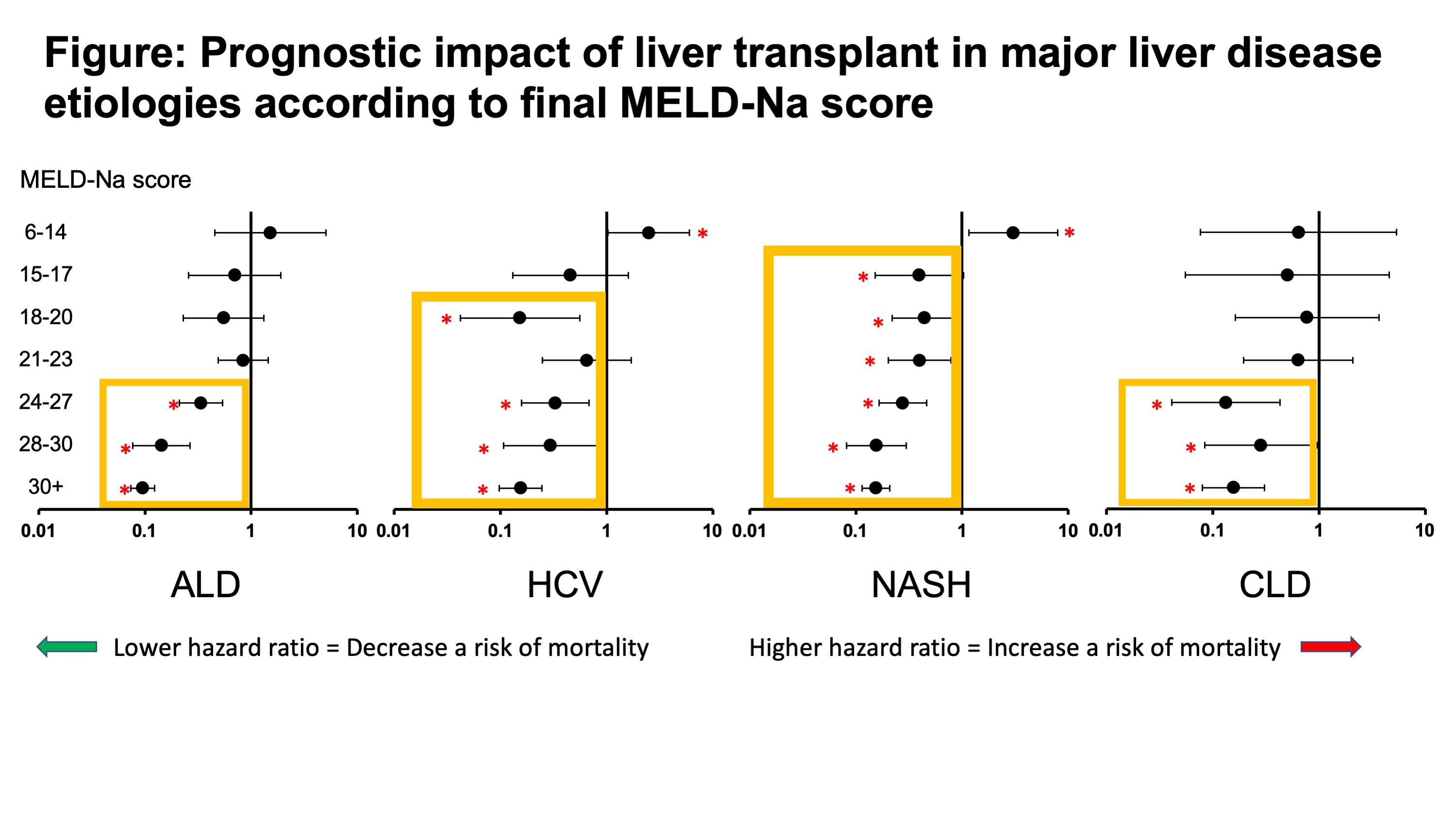
*Results: During the study period, 13016 patients listed for LT were selected in the study cohort, of whom 6094 had ALD, 1653 had HCV, 3848 had NASH, and 1421 had CLD. Of these patients, LT was performed in 3127 (51.3%), 816 (49.4%), 1893 (49.2%), and 644 (45.3%), respectively. In comparison with ALD patients, NASH patients had significantly higher risk of waitlist mortality (HR 1.32, p<0.001), whereas HCV (HR 1.14, p=0.09) and CLD (HR 1.00, p=0.99) patients showed similar risk. 90-day and 1-year post-transplant patient survival was significantly worse in NASH patients than those with ALD or CLD (90-day: P=0.025 and 0.064, 1-year: P=0.028 and 0.015). When assessing intention-to-treat survival, positive prognostic impact of LT was significant in MELD-Na score category of 24-27 in ALD (HR 0.338, P<0.001), score of 18-20 in HCV (HR 0.153, P=0.004), score of 15-17 in NASH (HR 0.441, P=0.021), and score of 24-27 in CLD (HR 0.283, P=0.042).
*Conclusions: Different thresholds of MELD-Na scores providing positive prognostic impact of LT were observed, which were higher in ALD and CLD patients and lower in NASH patients. Optimal timing of LT may be different among liver disease etiologies.
To cite this abstract in AMA style:
Nagai S, Kitajima T, Yeddula S, Moonka D, Collins K, Rizzari M, Yoshida A, Abouljoud M. Different Prognostic Impact of Liver Transplantation According to Liver Disease Etiologies [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/different-prognostic-impact-of-liver-transplantation-according-to-liver-disease-etiologies/. Accessed January 6, 2026.« Back to 2020 American Transplant Congress