Effect of Therapeutic Plasma Exchange on Glomerular Filtration Rate in Patients with Acute Humoral Rejection
Nephrology and Transplant Division, CMN 20 de Noviembre, Ciudad de Mexico, Mexico
Meeting: 2020 American Transplant Congress
Abstract number: A-022
Keywords: Antibodies, Efficacy, Hispanic, Plasmapheresis
Session Information
Session Name: Poster Session A: Kidney Acute Antibody Mediated Rejection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: AMR is the main risk factor for graft loss, especially after the first post transplant year. Up to 80% of patients achieve response with immunosuppressive treatment and TPE, although the response is lower in patients with late AMR. The objective was to determine the effect of TPE on GFR at 0, 1 and 3 months postTPE.
*Methods: Retrospective study that included patients with renal transplant of the CMN“November 20”ISSSTE from 2016to2019, undergoing membrane TPE for AMR. Analysis was performed using student’s t or MannWhitneyU, repeated measures analysis and Spearman or Pearson test. Significant p was less than 0.05.
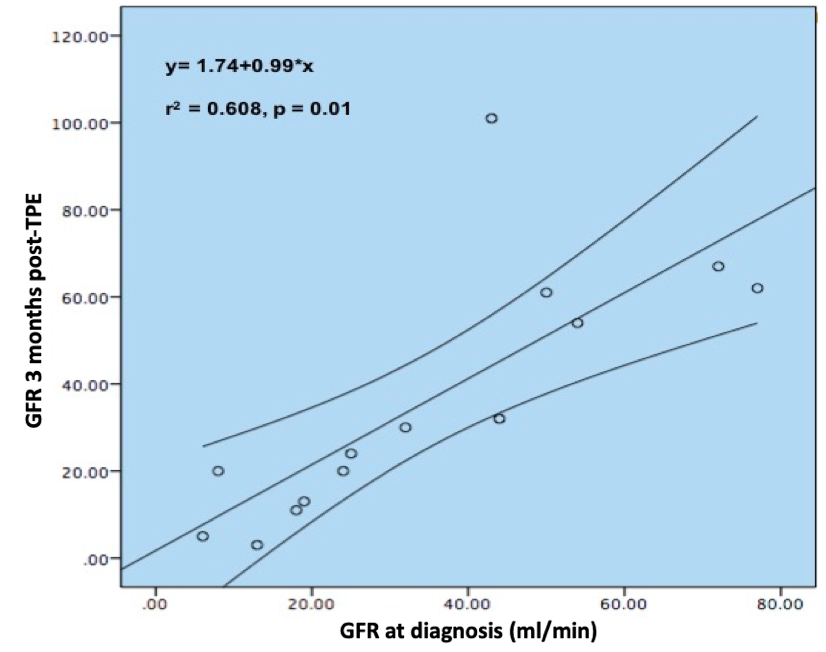
*Results: 25 patients with AMR who received TPE were evaluated. Age:32±11.6 years, 72% from living donor, and 52% received Basiliximab. 87% received tacrolimus. 80% of AMR events were late (more than 6 months post-transplant). The GFR at the time of diagnosis was38.2±23.8 ml/min, and at discharge (0), 1 and 3 months postTPE were 43.3±24.8, 34.1±19.5, and 35.9±28.7 ml/min. Prevalence of HLA class II DSA(66%), specifically vs DQ and DR (57.2% and 28.8%). There was a significant difference between preTPE GFR and at the end of treatment(p=0.015, r=0.53). There were no significant differences when comparing the preTPE GFR, with one monthGFR(p=0.58), or after 3 months postTPE(p=0.36). When evaluating IFTA, no difference was detected in the GFR at 3 months postTPE. When analyzing the histological score(g+ptc), no differences were detected between the score obtained and the average GFR at discharge(p=0.19), one month(p=0.22) and 3 months(p=0.06) post-TPE. When comparing the effect of the AMR temporality on the GFR, difference was found at one month (p=0.01) and 3 months (p=0.022) postTPE, with a lower recovery of GFR in patients with early AMR. The response to treatment(GFR±30% from baseline at 7 days postTPE) was 60%. There was a moderate correlation between GFR at the time of diagnosis of rejection and GFR at 3 months postTPE(r2=0.68,p=0.01).
*Conclusions: Significant difference was demonstrated between the preTPE GFR and the immediate postTPE GFR. IFTA did not appear to influence the GFR at 3 months. In our study patients with early AMR presented a poor response to treatment. The GFR upon admission correlated positively with the GFR detected at 3 months post-TPE. This suggests a beneficial effect of TPE over GFR fall during the first 3 months after diagnosis.
To cite this abstract in AMA style:
Moreno MMaza, Hernandez-Estrada S, Cervantes JCano, Tapia DMaldonado, Sanchez MAlamilla. Effect of Therapeutic Plasma Exchange on Glomerular Filtration Rate in Patients with Acute Humoral Rejection [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/effect-of-therapeutic-plasma-exchange-on-glomerular-filtration-rate-in-patients-with-acute-humoral-rejection/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress