Post- Transplant Recurrence of IgA Nephropathy: HLA as a Predictive Factor
1Pediatric Nephrology, Columbia University Medical Center, New York, NY, 2Pathology, Columbia University Medical Center, New York, NY, 3Surgery, Columbia University Medical Center, New York, NY
Meeting: 2020 American Transplant Congress
Abstract number: 618
Keywords: Graft survival, HLA matching, Kidney, Recurrence
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes VI
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:27pm-3:39pm
Presentation Time: 3:27pm-3:39pm
Location: Virtual
*Purpose: Genomic studies have identified several HLA antigens to be associated with IgA Nephropathy in the native kidney. In contrast to the native kidney, there is still limited knowledge of factors that contribute to recurrent IgA Nephropathy in the kidney allograft. Therefore, further evaluation is required to determine if the degree of HLA matching and the presence of certain HLA antigens in the donor and recipient can contribute to recurrence of IgA Nephropathy.
*Methods: Graft biopsies performed between 2005-2017 at Columbia University were reviewed. A total of 158 patients with the native disease of IgA Nephropathy were identified. Clinical characteristics as well as HLA typing were analyzed in both donor and recipient.
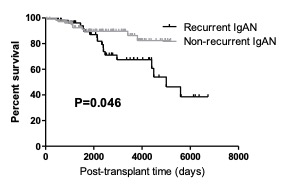
*Results: Of the 158 patients identified, 53 (33%) were found to have biopsy proven recurrence of IgA Nephropathy. Younger age at the time of transplantation (HR 0.95 [95% CI [0.93- 0.98], P= 0.002) was found to be an independent risk factor for recurrence. Recipient race and induction regimen were not significant determinants. No significant variation in recurrence rate was observed in living donors as compared to cadaveric donors. However, fewer HLA mismatches (HR 0.76 [0.62- 0.94], P=0.009) was independently associated with increased risk of recurrence. The presence of HLA DR15 in the recipient (HR 2.45 [1.27- 4.73], P= 0.009) as well as HLA DR3 in the donor (HR 2.80 [1.30 – 6.04], P= 0.008) were also found in increased frequency in those with recurrent disease. Of the 53 with biopsy proven recurrence, 16 (30%) were found to have graft failure. Recurrence in the graft was found to have significant impact resulting in decreased graft survival as compared to patients without recurrent disease (P= 0.046.)
*Conclusions: Recurrence of IgA Nephropathy was found to be associated with decreased graft survival. Thus, in an effort to prolong graft survival, it is imperative to take into account factors that increase recurrence risk when evaluating potential donors. The presence of fewer HLA mismatches, donor HLA DR3, and recipient HLA DR15 were associated with recurrent disease.
To cite this abstract in AMA style:
Kavanagh CR, Jain NG, Vasilescu R, Kamal J, Batal I. Post- Transplant Recurrence of IgA Nephropathy: HLA as a Predictive Factor [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/post-transplant-recurrence-of-iga-nephropathy-hla-as-a-predictive-factor/. Accessed February 3, 2026.« Back to 2020 American Transplant Congress