Comparison of Specificity and Sensitivity of Clinical Viability Criteria to Assess Transplantability of High-Risk Donor Livers
1Liver Unit, Queen Elizabeth Hospital, Birmingham, United Kingdom, 2Department of Statistics, Queen Elizabeth Hospital, Birmingham, United Kingdom, 3Centre for Liver and Gastroenterology Research, University of Birmingham, Birmingham, United Kingdom, 4Liver Unit, Darius Mirza, Birmingham, United Kingdom
Meeting: 2020 American Transplant Congress
Abstract number: 592
Keywords: Donors, marginal, Liver preservation, Machine preservation
Session Information
Session Name: All Organs: Organ Preservation/Ischemia Reperfusion Injury
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:51pm-4:03pm
Presentation Time: 3:51pm-4:03pm
Location: Virtual
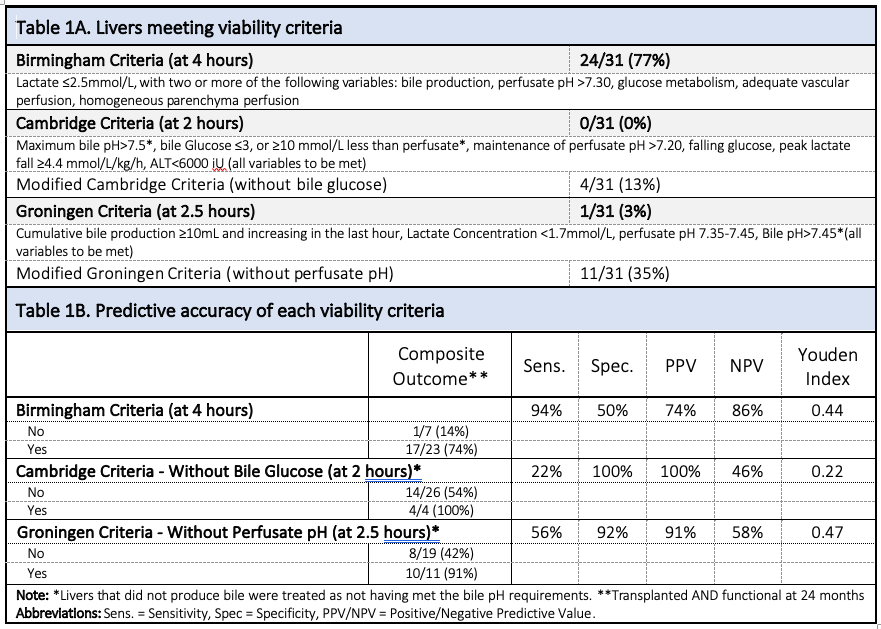
*Purpose: Normothermic machine perfusion (NMP) of the liver allows objective assessment before transplantation. To date, Birmingham (BC), Cambridge (CC) and Groningen Criteria (GC; Table 1A) teams have all introduced their own viability criteria.
*Methods: We applied these criteria separately to a cohort of 31 discarded livers tested by NMP following a variable period of cold storage to assess differences in organ utilisation and a composite outcome defined as graft functioning at 24 months, considering liver discard or graft failure as negative outcome.
*Results: Out of 31 livers, 24 (77%) met BC, whilst no (0%) livers met CC and only 1 (3%) liver met GC. 29% failed CC and GC because of absence of bile production. Removing the bile glucose component from CC (modified CC) meant 4 (13%) were considered viable, whilst excluding perfusate pH from GC (modified GC) increases the viability rate to 11 (35%). 22 (71%) livers were transplanted, of which all (100%) were functional at day 90. After excluding one liver with hepatic artery thrombosis, 18/21 (82%) of the remainder were functional at 2 years. The composite outcome was achieved in 74% vs. 14% of organs meeting vs. not meeting BC, yielding high sensitivity (94%) but poor specificity (50%; see Table 1B). All four organs meeting the modified CC had positive outcomes, giving 100% specificity; however, 54% of those that failed the criteria had a positive outcome, giving poor sensitivity (22%). A total of 91% (10/11) meeting the modified GC had a positive outcome, giving high specificity (92%), with a moderate sensitivity (56%). All graft failures were observed in grafts donated after circulatory death (DCD), due to non-anastomotic biliary strictures.
*Conclusions: This study suggests that some current viability criteria limit organ utilisation rates and removing the most restrictive variables may improve this without compromising outcome. Consideration of bile biochemistry might lead to liver underutilisation; however, it may prevent futile transplantations with DCD grafts.
To cite this abstract in AMA style:
Mergental H, Hodson J, Laing RW, Boteon YL, Attard J, Wallis L, Schlegel A, Muiesan P, Abradelo M, Perera MP, Mirza D, Afford SC. Comparison of Specificity and Sensitivity of Clinical Viability Criteria to Assess Transplantability of High-Risk Donor Livers [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/comparison-of-specificity-and-sensitivity-of-clinical-viability-criteria-to-assess-transplantability-of-high-risk-donor-livers/. Accessed February 5, 2026.« Back to 2020 American Transplant Congress