Socio-Demographic Disparities in Access to Organs from HCV-Viremic Donors among HCV-Negative Patients
1Medicine, University of Miami, Miami, FL, 2Massachusetts General Hospital, Boston, MA, 3University of Pennsylvania, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: 485
Keywords: Heart/lung transplantation, Hepatitis C, Kidney/liver transplantation
Session Information
Session Name: All Organs: Disparities to Outcome and Access to Healthcare II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:27pm-3:39pm
Presentation Time: 3:27pm-3:39pm
Location: Virtual
*Purpose: The success of pilot trials of transplanting organs from hepatitis C virus (HCV) viremic donors into HCV-negative recipients (HCV D+/R-) has led to an expansion of this practice. DAA therapies remain costly, and insurance barriers to approval remain, especially with HCV D+/R- transplantation due to the off-label nature of treating acute HCV after intentional HCV transmission. It is unknown if socio-demographic disparities exist with respect to access to HCV D+ organs among HCV-negative patients.
*Methods: We used OPTN/UNOS data from 1/1/17-6/30/19. We included kidney, liver, heart, and/or lung recipients transplanted at a center that performed ≥10 HCV D+/R- transplants of that organ type. A state’s HCV Medicaid policies were categorized as Grades A-F according to the Center for Health Law and Policy Innovation of Harvard Law School and the National Viral Hepatitis Roundtable. Hispanics and blacks were categorized as “under-represented minorities.” We fit multivariable mixed effects logistic regression models (center as random effect) to evaluate factors associated with receiving an HCV D+/R- transplant. We used marginal standardization to predict the standardized proportion of HCV D+/R- recipients within insurance and state sub-groups standardized with respect to the distribution of all other covariates.
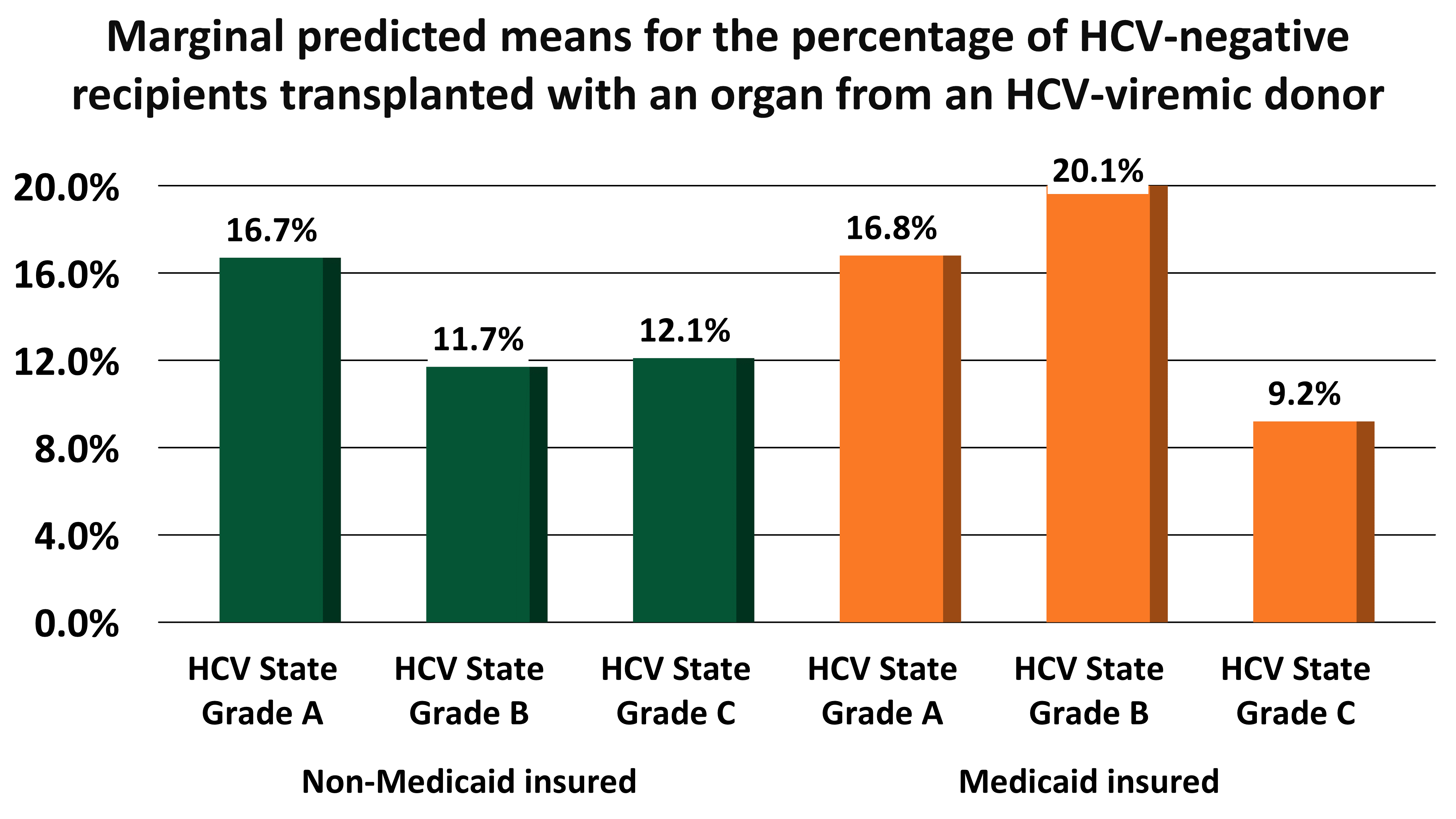
*Results: During the study period, 29 transplant centers performed ≥10 HCV D+/R- transplants of one organ type. In multivariable mixed effects models, women (OR: 0.70, 95% CI: 0.61-0.80, p<0.001) and under-represented minorities (OR: 0.80, 95% CI: 0.69-0.92, p=0.003) were significantly less likely to receive an HCV D+/R- transplant. Patients with an education level of grade school or less were significantly less likely to receive an HCV D+/R- transplant (OR: 0.55, 95% CI: 0.39-0.79 compared to college-educated; p=0.001). There was a significant interaction with Medicaid insurance and state HCV Medicaid grade (p=0.01), such that Medicaid insurance was only associated with a lower probability of receiving an HCV D+/R- in HCV Medicaid-restricted states (Figure).
*Conclusions: Women, under-represented minorities, patients with the least educational attainment, and Medicaid-insured patients living in HCV Medicaid-restricted states have less access to transplantation from HCV-viremic donors. Understanding the individual factors and public policies that contribute to the disparities in the transplant waitlist can aid in optimizing fair distribution of these limited resources.
To cite this abstract in AMA style:
Nguyen T, Williams W, Sise M, Reese P, Goldberg D. Socio-Demographic Disparities in Access to Organs from HCV-Viremic Donors among HCV-Negative Patients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/socio-demographic-disparities-in-access-to-organs-from-hcv-viremic-donors-among-hcv-negative-patients/. Accessed January 8, 2026.« Back to 2020 American Transplant Congress