Successful Tacrolimus Withdrawal in Kidney Transplant Recipients Unleashes a Peripheral Blood Transcriptional and Functional Signature Resembling Exhaustion
Icahn School of Medicine at Mount Sinai, New York, NY
Meeting: 2020 American Transplant Congress
Abstract number: 309
Keywords: Immunosuppression, Kidney transplantation, T cell reactivity
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes III
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:51pm-4:03pm
Presentation Time: 3:51pm-4:03pm
Location: Virtual
*Purpose: Tacrolimus (Tac) is an effective anti-rejection drug in kidney transplant recipients (KTR), but its off-target effects make withdrawal desirable. Studies indicate that Tac can be withdrawn in a subset of KTR, but the immune mechanisms that drive successful vs. unsuccessful Tac withdrawal are unknown.
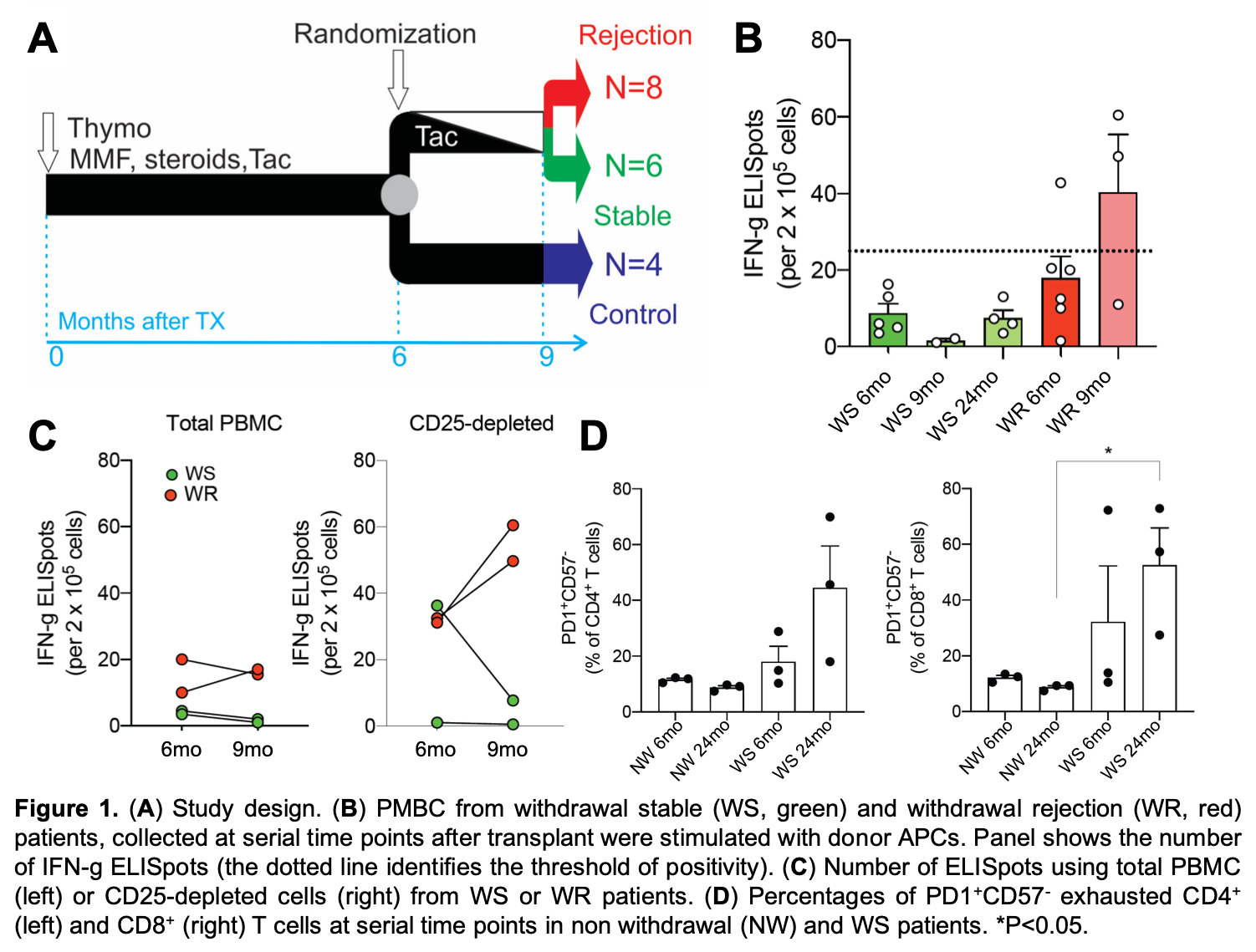
*Methods: We performed microarray analyses of peripheral blood mononuclear cell (PBMC) RNA samples from 18 KTR enrolled in the Clinical Trials in Organ Transplantation (CTOT)-09 study, in which stable patients were randomized to withdraw or continue Tac immunosuppression (Figure 1A). Samples were collected before (6mo post-tx), at the end of Tac withdrawal (9mo post-tx) and 12-18 mo post-tx. We also measured donor-reactive T cells (IFN-g ELISPOT, with and without CD25+ regulatory T cell depletion) and CD4+ and CD8+ T cells for PD1/CD57 expression by flow cytometry as a measure of exhaustion.
*Results: Analysis of differentially expressed genes (DEG) before vs. immediately after Tac withdrawal in subjects who developed acute rejection or donor-specific antibodies (withdrawal rejection, WR, n = 8) revealed upregulation of genes involved in immune activation. DEGs of PBMC RNA from those who successfully weaned Tac (withdrawal stable, WS; n = 6) enriched for downregulation of immune activity and upregulation of apoptosis. CellCODE analyses of gene expression data showed that within the WS subjects, both the downregulation of the T cell activation transcriptional program and upregulation of the apoptotic program following Tac withdrawal were preferentially confined to CD4+ and CD8+ T cells. Functional analyses of PBMCs suggested stronger donor-reactive T cell responses in WR vs WS without evidence of Tac-induced regulatory T cell dysfunction (Figure 1B-C). Flow cytometry of PBMC from the WS group show higher frequencies of exhaustion marker+ T cells up to 18 mo after Tac withdrawal compared to controls who remained on Tac (no withdrawal, NW; Figure 1D).
*Conclusions: Our data support the hypothesis that successful Tac withdrawal in KTRs can unleash an active, protective T cell program with features of exhaustion.
To cite this abstract in AMA style:
Cravedi P, Fribourg M, Harztell S, Anderson L, Heeger P. Successful Tacrolimus Withdrawal in Kidney Transplant Recipients Unleashes a Peripheral Blood Transcriptional and Functional Signature Resembling Exhaustion [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/successful-tacrolimus-withdrawal-in-kidney-transplant-recipients-unleashes-a-peripheral-blood-transcriptional-and-functional-signature-resembling-exhaustion/. Accessed February 9, 2026.« Back to 2020 American Transplant Congress