10-Year Experience Transplanting Very Highly Sensitized Patients with End Stage Renal Disease
J. Diaz1, J. Kennedy2, S. Chinnakotla3, P. Verghese4
1Department of Surgery, University of Minnesota, Saint Paul, MN, 2University of Minnesota, Minneapolis, MN, 3Department of Surgery, University of Minnesota, Minneapolis, MN, 4Department of Pediatrics, Division of Pediatric Nephrology, University of Minnesota, Minneapolis, MN
Meeting: 2020 American Transplant Congress
Abstract number: 201
Keywords: Donors, unrelated, Graft survival, Kidney, Survival
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:39pm-3:51pm
Presentation Time: 3:39pm-3:51pm
Location: Virtual
*Purpose: Very highly sensitized (VHS) individuals (calculated reactive antigen (cPRA) ≥ 95%) have increased rejection risk which negatively impacts kidney transplant outcomes. Multiple strategies have been utilized to offer this challenging population successful kidney transplant including priority on the deceased donor (DD) list via the new kidney allocation system (KAS), media appeals, participation in kidney paired donation (KPD), as well as desensitization therapy.
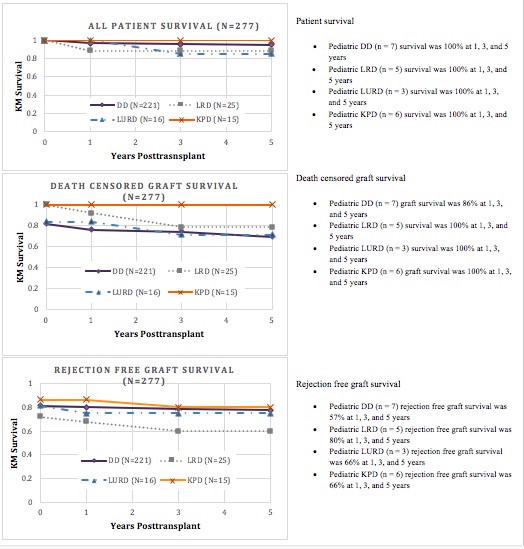
*Methods: In this retrospective single-center study, we evaluate KT outcomes in VHS recipients and compare the outcomes of DD, living related (LRD), KPD and living-unrelated (LURD) at the University of Minnesota since the beginning of the University of Minnesota’s Paired Exchange Program (PEP) in 2009 (N=277). We also present subgroup analysis in VHS pediatric kidney transplant recipients. Patient and graft survival curves at 0, 1, 3, and 5 years were compared using Kaplan-Meier survival analysis.
*Results: Of the 256 adult recipients, 221 were DD (death by cardiac death (DCD) n=27, brain-dead heart-beating donor (DBD) n=194), 16 LRD, and 40 LURD (non-KPD LURD n=15, KPD LURD n=25). Etiology of renal disease, gender, race, recipient age at the time of transplant, need for dialysis, mean cPRA, donor age, and donor-recipient age difference were similar across all groups. Zero were ABO mismatched. Time waitlisted was 0.3-164 months (mean 36 months, SD=32) with the longest times observed in DD and KPD, 38 and 35 months respectively. 65% (n=179) of the cohort had previously been transplanted. Cold ischemia time (CIT) ranged from 19-1924 minutes (mean 865, SD 417) with DD and KPD experiencing the longest CIT, 995 minutes and 523 minutes respectively. 27% of all recipients (n=76) received zero mismatched loci. Graft and patient survivals are summarized in figure 1.
*Conclusions: In our center, we observed improved patient and graft survival outcomes as well as rejection free survival in the KPD cohort. Although KPD CIT and time waitlisted in KPD was most similar to DD, KPD outcomes were superior to that of LRD outcomes. We hypothesize that KPD improves the ability to achieve superior HLA matching. The pediatric subgroup analysis suggest that LRD exhibit superior overall outcomes.
To cite this abstract in AMA style:
Diaz J, Kennedy J, Chinnakotla S, Verghese P. 10-Year Experience Transplanting Very Highly Sensitized Patients with End Stage Renal Disease [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/10-year-experience-transplanting-very-highly-sensitized-patients-with-end-stage-renal-disease/. Accessed February 28, 2026.« Back to 2020 American Transplant Congress