Impact of Immunogenicity on Kidney Allograft Survival in Patients Treated with Induction Therapy
University of Toledo, Toledo, OH
Meeting: 2020 American Transplant Congress
Abstract number: 105
Keywords: HLA matching, Induction therapy, Kidney transplantation
Session Information
Session Name: Histocompatibility and Immunogenetics
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:39pm-3:51pm
Presentation Time: 3:39pm-3:51pm
Location: Virtual
*Purpose: The induction therapy is currently used in the majority of kidney transplant recipients, regardless of their level of donor/recipient compatibility. We examined whether lower immunogenicity (IM) between donor and recipient improved allograft survivals in groups of recipients treated with three different induction therapies or without induction.
*Methods: We analyzed 30,648 deceased kidney transplants from 2009 to 2011 (SRTR database): 25,528 were with induction, namely 14,675 with anti-thymocyte globulin (equine or rabbit, ATG), 4,139 with anti-CD52 mAb (alemtuzumab, Alem), 6,714 with interleukin-2 receptor inhibitor (basiliximab, IL2-RI), whereas 5,120 remained without any induction. HLA-A/B/DR of donors and recipients were imputed from 2-digit to 4-digit HLAs by HaploStats algorithm. Each donor/recipient pair’s immunogenicity (IM) was then estimated by the Kosmoliaptsis algorithm, namely electrostatic mismatch score (EMS); pairs with IM scores above median (50th percentile) were considered as high EMS IM and below as low EMS IM.
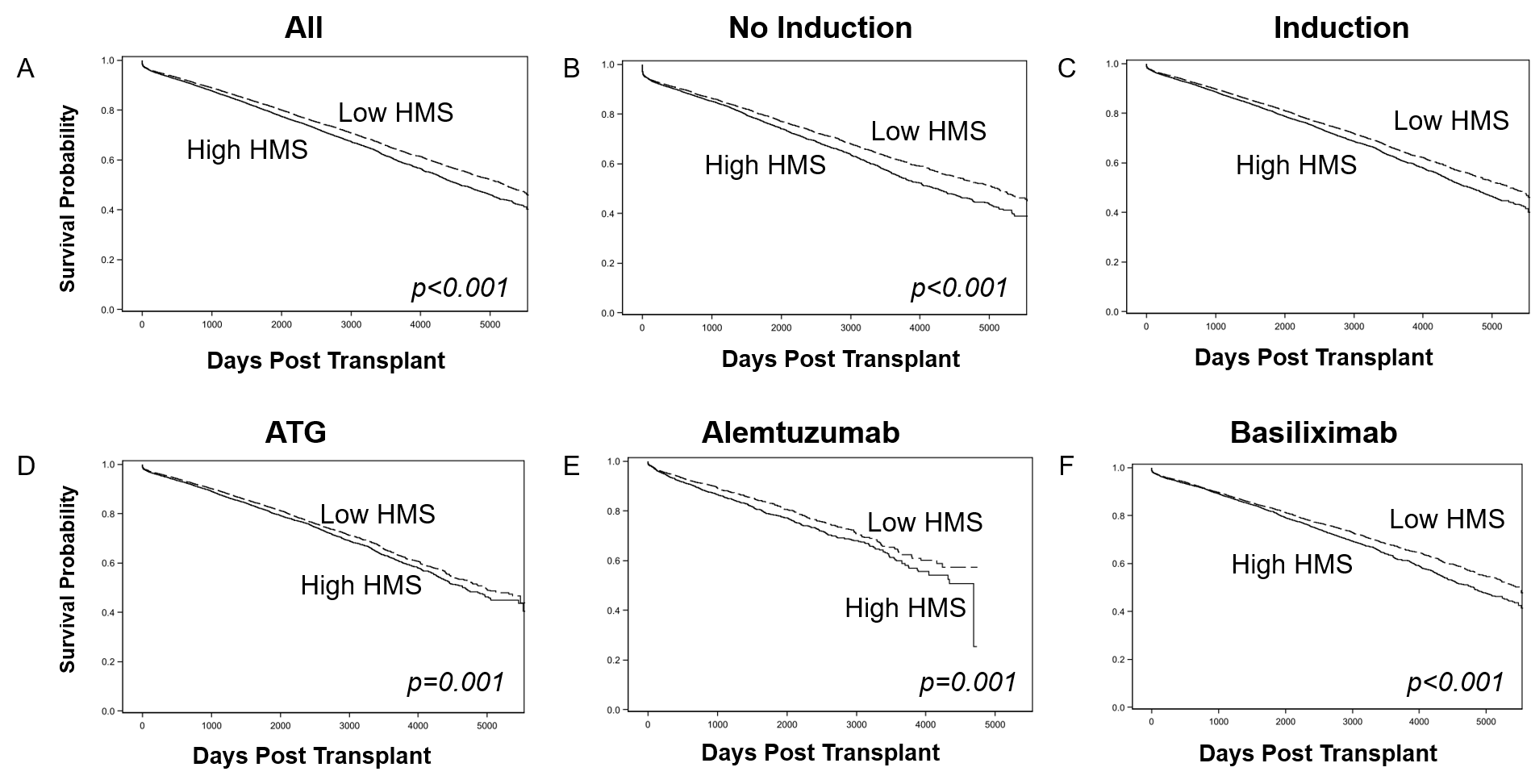
*Results: The 5-year death-censored graft survival for all induction groups combined was better than without induction (p <0.001; Fig. 1A); each of three induction groups (ATG, Alem, IL2-RI) was also superior to no induction (p <0.001; not shown). When no induction group (Fig. 1B), all induction groups combined (Fig. 1C), and each of the induction groups (ATG, Fig. 1D; Alem, Fig. 1E; and IL2-RI, Fig. 1F) were stratified by IM (EMS), there was a significant difference in the survival between low and high EMS groups (p <0.05; except of Alem, p=0.14). High and low IM groups for each induction therapy had the same distribution of HLA-A/B/DR mismatches: i.e. more pairs with 0-3 mismatches and less pairs with 5/6 mismatches in low IM groups vs. less pairs with 0-3 mismatches and more with 5/6 mismatches in high IM groups.
*Conclusions: 1) Independently of the induction protocol low EMS IM donor/recipient pairs display better graft survival than high EMS IM pairs; 2) Selection of low IM donor/recipient pairs by EMS may improve long-term kidney allograft survivals; and 3) 5/6 HLA mismatches have low IM pairs.
To cite this abstract in AMA style:
Michael R, Mierzejewska B, Bekbolsynov D, Ortiz J, Ekwenna O, Stepkowski S. Impact of Immunogenicity on Kidney Allograft Survival in Patients Treated with Induction Therapy [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-immunogenicity-on-kidney-allograft-survival-in-patients-treated-with-induction-therapy-2/. Accessed March 7, 2026.« Back to 2020 American Transplant Congress