Kidney Paired Donation Outcomes among High PRA Recipients
1University of North Carolina, Chapel Hill, NC, 2Johns Hopkins, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: 26
Keywords: Kidney transplantation, Sensitization
Session Information
Session Name: Kidney Paired Exchange
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Kidney paired donation (KPD) accounts for an increasing amount of living donor transplants in the US. Previous studies have shown equivalent outcomes between transplants facilitated by the National Kidney Registry (NKR), the largest US KPD clearinghouse, and non-NKR recipients. However, these studies did not stratify by high panel-reactive antibody (PRA) status. High PRA recipients may receive additional benefits from KPD participation through increased access to transplantation and desensitization avoidance.
*Methods: We studied 54,496 living donor transplants (2/2008-12/2017), including 2,363 NKR transplants, using the Scientific Registry of Transplant Recipients (SRTR) linked with the NKR database. We estimated the adjusted hazard ratio (aHR) of death-censored graft failure (DCGF) and mortality using inverse probability of treatment weighted Cox regression stratified by PRA (0 vs. >79). Cox models adjusted for recipient factors (sex, African American race, Hispanic ethnicity, age, BMI>30, diabetes, hypertension, previous transplant, college education, public insurance, preemptive transplant, eGFR, induction, and year of transplant) and accounted for center-level effects.
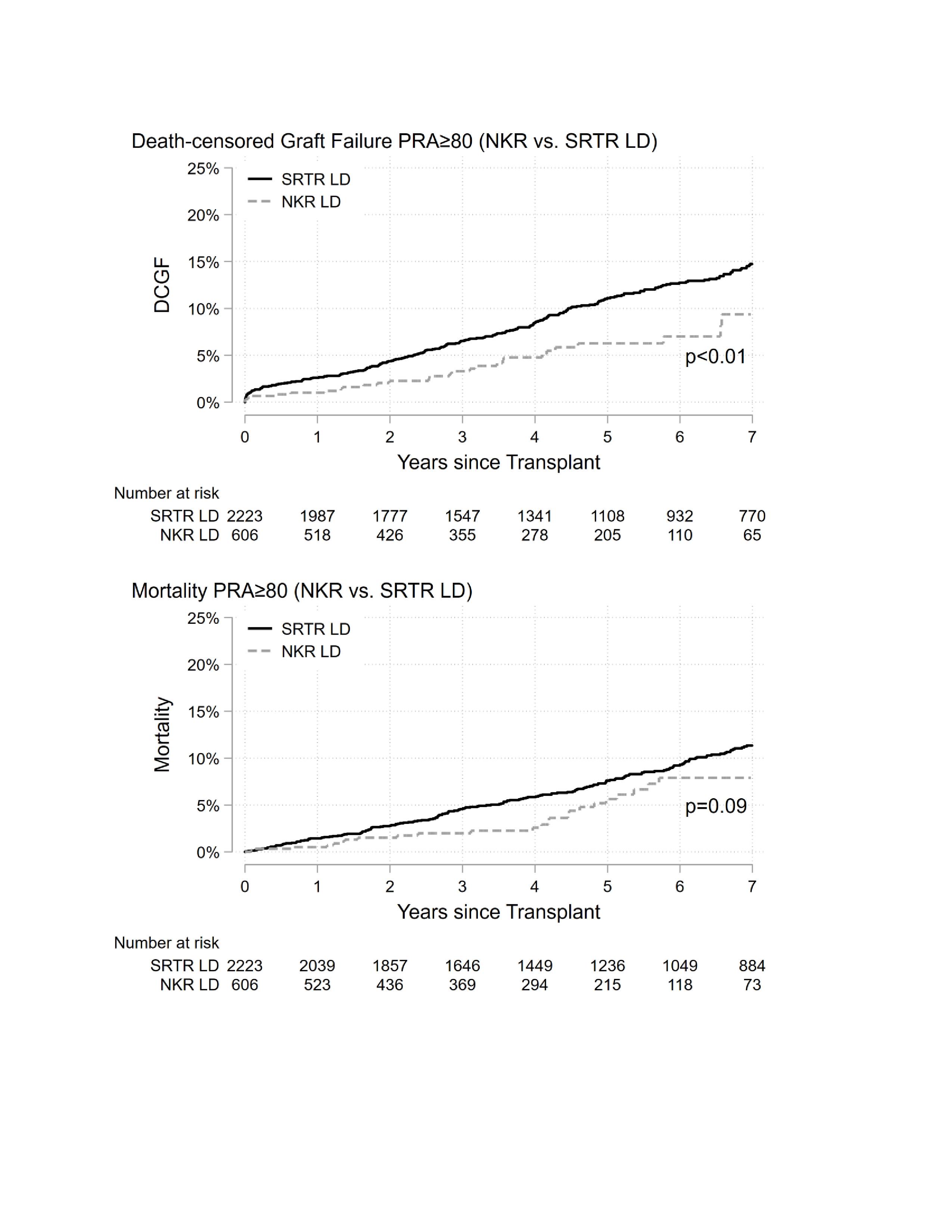
*Results: There were 40,847 zero PRA transplants (1,408 in NKR) and 2,829 high PRA (PRA>79) transplants (606 in NKR). Nearly half (n=294, 49%) of all high PRA NKR transplants were done at 10 centers (out 76 NKR centers). Among zero PRA recipients, there were no differences between NKR and non-NKR transplants for DCGF (p=0.3) or mortality (p=0.5). Among high PRA recipients, NKR-facilitated transplants had lower DCGF (aHR=0.68, 95% CI: 0.46-1.01, p=0.054) and mortality risk (aHR=0.56, 95% CI: 0.37-0.86), p<0.01). When models did not account for center-level effects, the log aHR standard deviation (sd) for DCGF (sd=0.14 vs. 0.19, F-test p<0.01) and mortality (sd=0.12 vs. 0.15, F-test p<0.01) increased suggesting greater between center than within center variation. Further adjustment for donor and transplant factors did not affect inferences.
*Conclusions: While outcomes among zero PRA recipients were similar, high PRA recipients experienced lower graft failure and mortality risk with NKR-facilitated transplants compared to non-NKR facilitated transplants. A small number of centers performed nearly half of all high PRA NKR transplants. Center-level factors, such as experience with high PRA patients, or desensitization (unmeasured) may partially explain the observed difference between NKR and non-NKR facilitated transplants. High PRA patients may benefit from entering a KPD system.
To cite this abstract in AMA style:
Thomas A, Shaffer A, Henderson M, Segev D. Kidney Paired Donation Outcomes among High PRA Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/kidney-paired-donation-outcomes-among-high-pra-recipients/. Accessed February 22, 2026.« Back to 2020 American Transplant Congress