Thymoglobulin (ATG) Induction vs. Campath vs. Simulect in DCD Kidneys in UK; Induction Regimes Play a Role after All
1Cardiff Transplant Unit,, University Hospital of Wales, Cardiff, United Kingdom, 2Infection and Immunity, Cardiff University, Cardiff, United Kingdom
Meeting: 2020 American Transplant Congress
Abstract number: 5
Keywords: Donors, non-heart-beating, Glomerular filtration rate (GFR), Induction therapy, Survival
Session Information
Session Name: Kidney Immunosuppression: Induction Therapy
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Controlled DCD kidneys have increased dramatically in UK. They suffer from a higher rate of DGF and, often in UK, come from older donors than DBD kidneys. 3C is the largest non commercial study of induction immunosuppression (Campath vs. Simulect) among all types of kidney transplants and has shown an advantage of Campath in terms of acute rejection but not graft survival. Aim of this study was to examine the effect of induction immunosuppression (ATG vs. Campath vs. Simulect) on the outcome of DCD kidneys.
*Methods: Raw data of the cohort of DCD patients (275) of the 3C study was obtained from the Sponsor. Prospectively collected data of the patients (140) who received ATG induction for DCD kidneys in a single centre (standard of care for DCD transplants in that centre) with the same entry criteria as the 3C were also included in the analysis, giving a total of 415 patients on the three induction regimes. Uncensored and censored for death graft survival at 6 months, 1 and 2 years was the primary outcome, acute rejection and MDRD eGFR were secondary outcomes. Analysis was performed by an independent statistician.
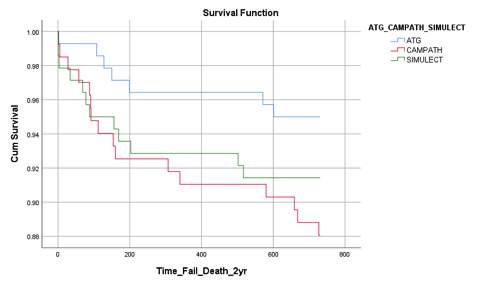
*Results: There were more male donors in the ATG group (70% vs. 59% in Campath, and 51% in Simulect, p<0.05) and more DR mismatched patients in the ATG group (82% vs 71.6% vs. 68%, p<0.05), with no difference in donor, recipient age, CIT. Adjusted, uncensored for death graft survival, was higher at 6 months and 1 year in the ATG compared to Campath group (95% CI of RR of failure or death for Campath vs ATG at 6 months was 0.86-8.7, p=0.08, and at 1 year 0.85-7.9, p=0.06). 2-year graft survival was 95% in ATG vs. 88% in Campath (p=0.036) and 91.5% in Simulect group (Figure 1).
Patients on ATG had better, censored for death, graft survival at 6 months compared to Simulect (p=0.057) but not compared to CAMPATH (p = 0.29). Acute rejection was 17% in the Simulect vs. 4.3% in ATG and 6% in Campath group (p<0.001). Donor age >60 (p<0.001), acute rejection (p<0.001), CIT >15hours (p=0.052) but not induction were significant for the eGFR at 6 months and 2 years.
*Conclusions: ATG induction in DCD transplants provides an advantage over Campath in terms of uncensored for death graft survival and provides the same advantage as Campath over Simulect in terms of acute rejection.
To cite this abstract in AMA style:
Asderakis A, Sabbah T, Watkins J, Szabó L, Elker D, Ilham AM, Ablorsu E, Stephens M, Khalid U, Chavez R. Thymoglobulin (ATG) Induction vs. Campath vs. Simulect in DCD Kidneys in UK; Induction Regimes Play a Role after All [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/thymoglobulin-atg-induction-vs-campath-vs-simulect-in-dcd-kidneys-in-uk-induction-regimes-play-a-role-after-all/. Accessed February 5, 2026.« Back to 2020 American Transplant Congress