The Rapidly Aging Population of Liver Transplant Patients with Hepatocellular Carcinoma
Division of Gastroenterology & Hepatology, UCSF, San Francisco, CA
Meeting: 2019 American Transplant Congress
Abstract number: D362
Keywords: Age factors, Hepatocellular carcinoma
Session Information
Session Name: Poster Session D: Late Breaking
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Hepatocellular carcinoma (HCC) is the fastest rising cause of cancer-related mortality in the US and a leading indication for liver transplant (LT). Direct acting anti-HCV therapy (DAA) and the rising burden of NASH have led to the aging of the LT population – whether this differentially impacts HCC patients (pts) is unknown.
*Methods: Using UNOS/OPTN data, we analyzed all pts≥18y listed for LT from 2003-17. Pts were grouped by age at listing (<65y or ≥65y). Nonparametric tests and standardized regression coefficients were used to compare time trends between HCC and non-HCC pts, stratified by disease etiology. Cox regression associated HCC and age with post-LT mortality.
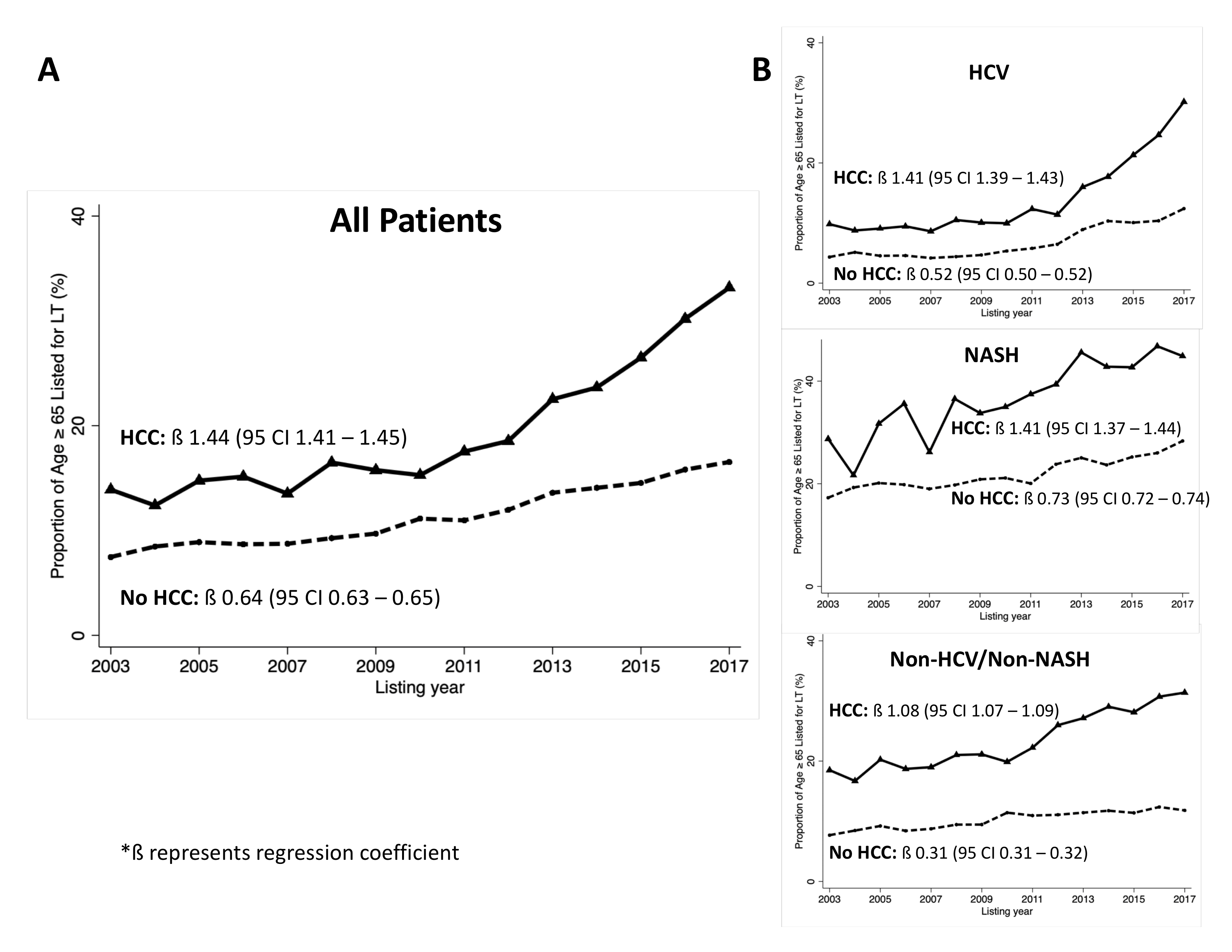
*Results: Included were 161,724 LT candidates: 14% were ≥65y at listing; 25% were listed with HCC exceptions. Among those without HCC, the %≥65y rose from 8% in 2003 to 17% in 2017 (ß=0.64, p<0.001); among those with HCC, the %≥65y rose from 14% in 2003 to 33% in 2017 (ß=1.44, p<0.001) (Figure 1A). Among pts with HCV, the %≥65y with HCC rose significantly more rapidly (ß=1.41, p<0.001) than in pts without HCC (ß=0.52, Δ=0.89, p<0.001). A similar trend was seen in those with NASH (Δ=0.68, p<0.001) and those with non-HCV/non-NASH cirrhosis (Δ = 0.77, p<0.001), though trend differences were smaller (Figure 1B).
Among all patients who underwent LT, in univariable regression, both HCC (SHR 1.13, 95CI 1.10-1.17) and age ≥65y (SHR 1.39, 95CI 1.33-1.44) were associated with increased mortality [p<0.001 for both]. In multivariable analysis, after adjustment for etiology, lab MELD, region, and donor risk index, both HCC (aSHR 1.16) and age ≥65y (aSHR 1.48) remained significantly associated with post-LT mortality (p <0.001 for both). Importantly, we observed a significant interaction between HCC and age ≥65y on post-LT mortality (p=0.04): among pts <65y, HCC conferred on average a 42% (30-54%) increased risk of post-LT mortality (p<0.001), but in those ≥65y, HCC did not confer any added risk 25% (-4-55%). Among pts with HCC who underwent LT, 1- and 5-year survival rates were similar for pts <65y (92% and 80%) and ≥65y (90% and 79%).
*Conclusions: The population of LT pts with HCC is rising at a rate that is over 2x faster than those without HCC – one-third of pts listed for HCC were ≥65y in 2017. This trend appears to be driven greatest by those with HCV and NASH. Although older age is associated with worse post-LT outcomes, our data suggest that the risk of age on post-LT mortality is significantly lower in HCC than non-HCC pts. Thus, the rapidly growing population of older adults with HCC may provide an opportunity for expanding LT access without compromising post-LT outcomes.
To cite this abstract in AMA style:
Rubin JB, Cullaro G, Mehta N, Lai JC. The Rapidly Aging Population of Liver Transplant Patients with Hepatocellular Carcinoma [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-rapidly-aging-population-of-liver-transplant-patients-with-hepatocellular-carcinoma/. Accessed March 2, 2026.« Back to 2019 American Transplant Congress